Abstract: Transversus abdominis plane (TAP) catheters are increasingly being used as an opioid-sparing analgesic technique following abdominal surgery. The aim of this systematic review is to evaluate the efficacy and safety of TAP catheters for postoperative analgesia following abdominal surgery in adults. The authors searched electronic databases and relevant reference lists for randomizedcontrolledtrials published between inception and January 2017. Twelve randomized controlled trials were identified,
comprising 661 participants, with several trials showing either an equiv alence or superiority in analgesia compared with the alternative modality. Because of the extremely heterogeneous nature of the studies, a
specific consensus regarding their results, or the ability to construct a meta-analysis, is unviable. Although there are promising indications for the benefit of TAP catheter techniques, extrapolation/comparison
of results and application to patient care will be better elucidated when there is more standardization of TAP catheter techniques and the meth odology for measuring efficacy.
(Reg Anesth Pain Med 2018;43: 5–13)
Pain following abdominal surgery can adversely affect postoperative recovery, potentially contributing to morbidity and mortality.1 For larger abdominal operations, epidural analgesia has long been used as a viable method for managing postoperative pain.2 The benefits of epidural analgesia are alongside a number of potential adverse effects, which have led to a broad adoption of alternate analgesic options.3
One increasingly popular regional anesthetic alternative is the single-shot transversus abdominis plane (TAP) block.4 An injection of local anesthetic into the fascial plane between the internal oblique and transversus abdominis muscles is used to achieve analgesia in the somatic dermatomal distribution of T7–L1, with variation depending on the technical approach.5 Transversus abdominis plane blocks do not provide visceral analgesia similar to epidural blockade,5,6 thus often requiring supplementation with
systemic analgesia.
A Cochrane review of TAP blocks versus placebo demonstrated limited evidence that TAP blocks reduce postoperative opioid requirements, and no comparison could be made of TAP blocks versus epidural analgesia based on 5 studies.7 A more recent meta-analysis of TAP blocks versus placebo dem on strated a significant reduction in visual analog scale (VAS) pain scores and morphine consumption,8 but a limiting factor of single-shot TAP blocks is a 24-hour maximum expected du ration of action.5
To prolong the TAP block, catheters are increasingly being inserted and trialed in a range of procedures, which otherwise might commonly favor epidural placement.9
To date, no systematic review of this topic has been published.10 This review will evaluate the comparative analgesic efficacy and safety that TAP catheters may provide.
This review protocol was published on the PROSPERO (International Prospective Register of Systematic Reviews 11) protocol and conforms to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) statement.12 The authors
independently searched the US National Library of Medicine database; MEDLINE (including MEDLINE In-Process); EMBASE (Excerpta Medica database); CENTRAL (the Cochrane Central Register of Controlled Trials); Cochrane Database of Systematic
Reviews for published studies and registries of ongoing trials; World Health Organization (http://apps.who.int/trialsearch/De fault.aspx); Clinical Trials.gov (http://clinicaltrials.gov); Current Controlled Trials; ISRCTN Registry (http://www.isrctn.com); and the Australian and New Zealand Clinical Trials Register (http://anzctr.org.au). Search terms included “transvers*,”“abdomin*,” “contin*,” “catheter*,” and explosion or mesh terms “nerve block” and “abdominal muscles,” where appropriate. The last electronic search was completed in January 2017. Bibliographies of relevant articles were screened for additional references, and studies were restricted to English language and those performed on humans. Both authors independently screened abstracts, with eligibility for inclusion assessed based on title and abstract and any disagreements regarding inclusion resolved by discussion. A flowchart of this process is shown in Figure 1.
The patient population was limited toadults (ages ≥18 years) undergoing abdominal surgery, in day-stay surgery or inpatient hospital settings. We excluded nonrandomized or quasi-randomized studies, retrospective studies, prospective observational studies, studies in volving pediatric patients (aged <18 years), and studies only com paring different types or doses of local anesthetic agent. Details of the intervention (TAP catheter) and comparators, including number of subjects per group and description of block technique, were sought from each study, along with the type of operative anesthesia. Analgesic outcome data were based on the recent review by Abdallah et al,13 with our primary outcome being pain scores (VAS scores) at 48 hours following surgery. Secondary outcomes were cumulative dose of postoperative rescue
analgesia, pain scores at 24 and 72 hours following surgery (both at rest and dynamic), time to first rescue analgesia, length of post operative hospital stay, opioid adverse effects (such as nausea and vomiting, sedation, pruritus), block complications, and patient satisfaction. Risk-of-bias assessment used the Cochrane tool for randomized trials.14
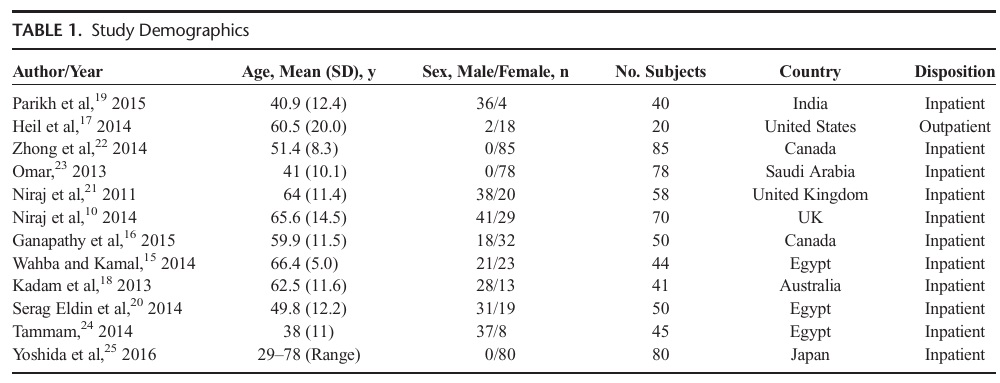
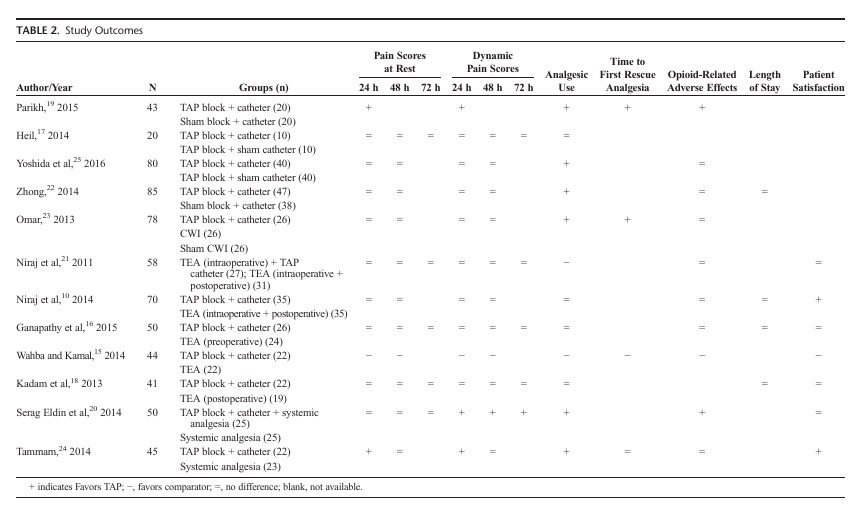
We identified 12 studies (11 from the database search and 1 from bibliographic review), comprising 661 subjects.10,15–23 Study characteristics are presented in Table 1 and with outcomes listed in Table 2.
Methodological Quality and Evidence of Bias
The overall risk of bias for the included trials was low (Fig. 2). Of the 12 included trials, only 4 trials 17,19,22,25 used par ticipant blinding, and only 6 trials 17,19,22–25 were blinded on outcome assessment. Publication of study protocols prior to trial commencement was inconsistent among the selected trials.
Efficacy
Overall
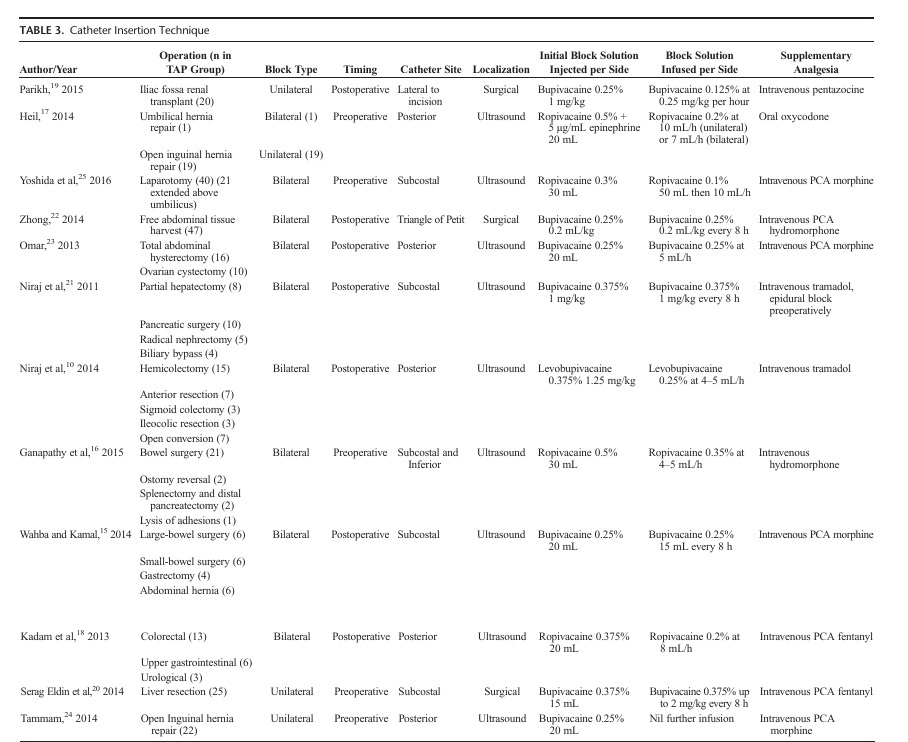
On initial review, we immediately identified a wide heterogeneity in the trials’ control modalities and supplementary analgesia regimens (Table 3).
Transversus abdominis plane catheters were evaluated against a range of surgical operations, with only 5 trials examining a single operation in all their participants.19,20,22,24,25 Four trials 17,19,22,25 compared
TAP catheters against placebo
TAP catheters:
One trial 19,22 found a significant reduction in 24-hour postoperative VAS scores, reduced opioid consumption, and mean delayed time to first analgesic request by 227 hours. Another trial demonstrated a 31% reduction in equianalgesic morphine consumption at 24 hours.22 A third placebo cathetertrial, where both groups received an initial TAP block, was able to demonstrate a reduced supplemental analgesic requirement by 43%.25 Transversus abdominis plane catheters were also compared
with continuous wound infusions (CWIs),23 demonstrating an in creased time to first morphine request by 2 hours compared with CWI and by 8 hours compared with placebo CWI. The same trial also demonstrated a 73% reduction morphine consumption using TAP catheters at 48 hours compared with placebo CWI.23 The
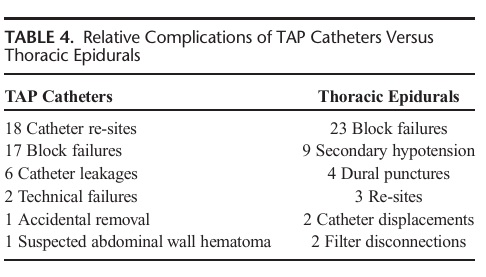
data regarding comparative efficacy of analgesia with TAP catheters have been summarized in Table 4.
Thoracic Epidural Analgesia Versus
TAP Catheters
Transversus abdominis plane catheters and thoracic epidural analgesia (TEA) were examined in 5 trials.10,15,16,18,21 Of the setrials, only 1 trial 10 demonstrated a significant analgesic benefit via improved patient satisfaction scores.
Patient-Controlled Analgesia and
TAP Catheters
Two trials examined TAP catheters against patient-controlled analgesia (PCA). Comparing fentanyl PCA and TAP catheters to fentanyl PCA alone 20 demonstrated that TAP catheters reduced VAS pain scores with movement by more than 20 mm
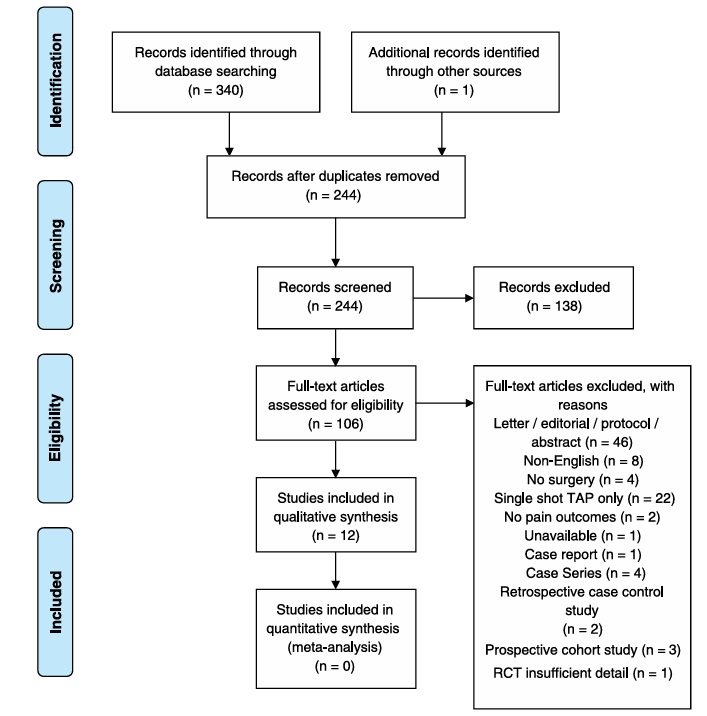
FIGURE 1. Flowchart of study selection (PRISMA).
at 24,48,and 72 hours and fentanyl consumption by 21 % and sedation by 29 % at 72hours.The remaining trial compared single-bolus TAP catheters and PCA morphine against PCA morphine alone.This comparison demonstrated a reduction in pain scores at rest and with cough by 1.5 and 3(out of 10),re spectively.24 This trial was also able to show that TAP catheters reduced supplemental morphine by 69 % at 48 hours and improved patient satisfaction.24
Technique
Significant heterogeneity in catheter insertion techniques was found between studies,summarizedin Table 3
Nine trials 10,15–18,21,23–25 utilized ultrasound and Tuohy needles for catheter insertion,with 5 trials 10,17,18,23,24 placing catheters via the posterior approach, 3 trials 15,21,25 via the subcostal approach, and 1 trial 16 via the subcostal/inferior approach to the abdominal wall.
Two studies comparing TAP catheters to TEA evaluated pro
cedural time for block placement (mean). Insertion of subcostal
andinferior TAP catheterspostoperatively (bilaterally) hadamean
timeof35.5minutes,16comparedwith14.7minutesforthoracic
epidural insertionpreoperatively. The second trial18 showeda
meantimeof 16.2 minutes for insertingbilateralposterior TAP
catheterspostoperatively, compared with 19.5 minutes for tho
racicepiduralsinsertedpreoperatively.
Three trials 19, 20 ,22 use dsurgicallyinserted TAP catheters at the end of the operation. One study 19 used a single catheter,lateral to the incision, showing superiority against placebo catheters. One study 22 that inserted TAP catheters into the triangle of Petit via a separate incision found TAP catheters superior to placebo catheters, reducing analgesia requirements by 31 % at 24 hours.The final trial 20 combined systemic analgesia with a single, subcostal, TAP catheter following liver resection. Compared with systemic analgesia alone, this study demonstrated superiority of TAP catheters by reduced VAS pains cores, a 21 % reduction in fentanyl consumption, and a 29 % reduction in sedation (attributed to opioid use).
Local Anesthetic Administration
The regimen for local anesthetic infusion via TAP catheters again showed significant heterogeneity. Four trials 15,20–22 used boluses at 8 hourly intervals. Seven other trials 10,16–19,23,25 administered local anesthetic by continuous infusion, ranging from 4 to 10 mL/h through each catheter.
Complications
Ten trials 10,16–22,24 reported complications associated with TAP catheters in 405 participants. In descending order of frequency, these complications were as follows:
• 18 catheter re-sites
• 17 block failures
• 12 catheter leakages
• 4 accidental removals
• 4 suspected intravascular placements
• 2 technical failures
• 1 catheter blockage
• 1 suspected abdominal wall hematoma
For the trials that reported complications in TAP catheter versus TEA,10,16,18,21 a total of 110 participants received TAP catheters compared with 109 participants with TEA. The associated complications are listed in Table 4. There were no reported episodes of local anesthetic systemic toxicity.
The collection of limited studies currently in publication paints a general picture that, in combination with systemican algesia, TAP catheters following abdominal surgery present another option for effective and safe extended analgesia. Evidence for superiority of TAP catheters, in terms of analgesia and effective duration, is still limited. All studies included in this review were randomized controlled trials; however, the small study populations and variable surgical procedures limited their power and ability to collectively demonstrate significant analgesic differences. One promising randomized controlled trial examined single-shot TAP blocks versus TAP catheters.This study demonstrated reduced VAS pain scores at 24 hours in the catheter group, but because of insufficient detail on its methodology and results,it was not included.26
A consistent confounding factor uncovered in this review is the extensive heterogeneity in study methods, procedural techniques, comparison analgesic modalities, and surgical populations.
This variability not only confounded our ability to make a
conclusive summative statement regarding the benefit of TAP
catheters, but also highlight show the term “TAP catheter” is used
to broadly describe a variety of techniques.
Surgical Population
A wide variety of surgical interventions and therefore surgical incisions were assessed against TAP catheters (Table 3). Although denoting only the somatic and not necessarily the visceral component of any surgical stimulation, we feel that an operative procedure being defined as simply “abdominal surgery” is too broad.
Likewise, acknowledging that the dermatomes/terminal branches covered by a TAP block/catheter are expected to fall within a specific range, generalizing their efficacy for “abdominal” surgery is also too broad.
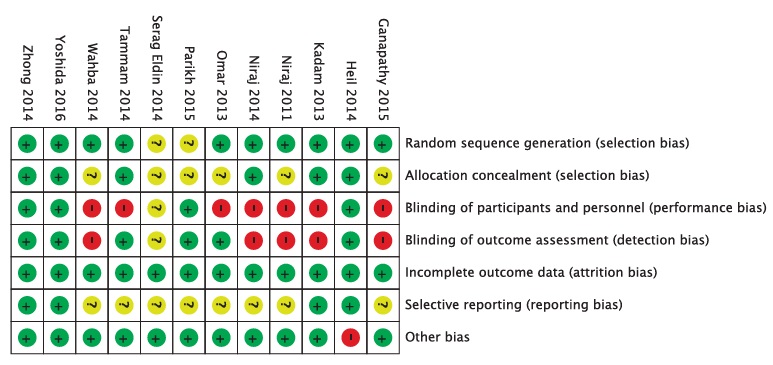
FIGURE 2. Risk-of-bias assessment for included trials.
Based on dye imaging and clinical studies, the evidence concerning the dermatomal coverage of TAP block is controversial where administration of local anesthetic in either the subcostal, lateral, or posterior region of the TAP has been shown to cover limited segments and the entire TAP plexus (T7–L1) or suggested to extend beyond to the paravertebral space.5,27–29 A more appropriate alternative may be for future studies to group surgical populations by the relevant abdominal quadrant (unilateral or bilateral) to allow for more accurate comparison be tween studies and improve clinical application to appropriate patient populations. Several studies demonstrated a benefit of TAP catheters (in addition to systemic analgesia) over systemic analgesia alone viareduced painscores, decreased supplemental an algesia, and a concomitant reduction in opioid adverse effects. While TAP catheters were evaluated as equianalgesic compared with TEA at 72 hours post operatively, the analgesic significance of the outcomes demonstrated by Parikh et al19 and Serag Eldin et al20 needs to betaken in context that these studies focused on a single surgicaloperation, involving incisions made through relatively limited abdominal dermatomes. This is compared with the study by Wahba and Kamal,15 who examined subcostal TAP catheters for abdominal operations covering a broad range of dermatomes. TAP Catheter Technique Although each study focused on a comparison of TAP catheters to a more conventional analgesic regimen, we feel that studies included the use of a TAP catheter in too binary an interpretation; it was either present or it wasn’t. The function and efficacy of a TAP catheter are affected by a variety of factors, many of which are still being elucidated in the scientific literature. As such, what constitutes using a TAP catheter was found to be markedly different from one study to another. This review demonstrates that the term “TAP block” (as a single-injection or catheter technique) is now used to describe a heterogeneously applied regional anesthetic technique. Logically, procedural variations (with subsequent effects on function) will confound the ability to draw accurate comparisons or conduct meta-analyses. In addition to the technical skill of placing a TAP block/catheter, the local anesthetic infusion protocols are equally diverse. While intermittent bolus and continuous infusion were common among the included trials, comparison between these methods has not been made in any 1 trial. Suchfactors as location of catheter, catheter size, depth of insertion, number of catheter ports, type of local anesthetic, method of local anesthetic infusion, and infusion versus bolus regimens are among the variables encountered in this review. This heterogeneous chain of variables underpins the difficulty in generalizing the use and efficacy of TAP catheters.
Until further characterization and standardization surrounding the techniques for TAP catheter use are developed, our ability to compare them, as a broad group, will be hindered.
Extrapolating from a recent randomized crossover study of continuous versus intermittent bolus protocols with posterior TAP catheters,30 evaluation of local anesthetic administration techniques over a longer period with higher volumes may identify an optimal infusion protocol, and as such, we encourage further research on this topic while considering risk profiles for toxicity.31 Assessment of Block Function Across most of the studies reviewed was a lack of objective assessment for block function. As opposed to the more obvious motor block observed with brachial plexus or femoral blocks, TAP blocks are more difficult to assess. As such, a predominance
of studies evaluated the analgesic benefit of these techniques, without validating successful establishment of the block as well. Considering the wide variety of insertion sites, techniques, and catheters used, the potential for how this may affect block success necessitates having an objective measurement of block function to genuinely compare and quantify the analgesic effect of a successful TAP block and/or catheter.
Supplementary Analgesia
While what each study considered to constitute the use of a TAP catheter was varied, there was equally awide heterogeneity in the types of supplementary analgesia included in their respective protocols.
Recalling that TAP catheters are predominantly expected to address the somatic component of surgical stimulation but not the visceral component, the supplementary analgesic regimen se lected may also have a significant effect on the overall degree of
analgesia achieved. Each study included in this review was found to use a differ ent supplemental analgesia protocol (Table 3). Translating each regimen into comparable units, such as morphine equivalents, is too simplistic (considering their variety of pharmacokinetics), further highlighting the difficulty in assessing and comparing the TAP catheter techniques used in these studies.
Complications and Management
The potential complications associated with the use of TAP catheters are similar to most other catheter techniques, namely, in fection, hematoma, or local anesthetic toxicity. Compared with neuraxial anesthesia, the morbidity from complications observed
with TAP catheters seems to be less severe. Practically, the care and maintenance of a TAP catheter protocol may be considered advantageous for institutions not staffed or structured to accom modate caring for postoperative epidurals or their potential com
plications (such as neurosurgical evaluation or intervention).32 Based on the reported complications of the included trials, TAP catheter analgesia should be considered a relatively safe tech nique, as only a single complication not related to technical failure
of the technique itself was reported. This review suggests that TAP catheters (in combination with systemic analgesia) have the potential to provide effective and safe
analgesia. Several studies demonstrated effects comparable to TEA, while showing consistent superiority to systemic analgesia alone, along with a comparatively more favorable adverse effect profile.9 Whereas one of the included studies only reported painscores up to 24hours, several studies demonstrated analgesic benefits up to 72 hours past the initiation of the catheter placement, supporting the extended benefit of TAP catheters over single shot blocks. The limited power of the included trials, potential
confounding by the broad range of abdominal surgeries, and the
heterogeneous nature of TAP catheter techniques used limit fur ther investigation by meta-analysis. In addition, a lack of objective testing for block success and a lack of ongoing monitoring for sensory block duration in most trials also limit evidence of efficacy because of potential confounding of an untested TAP catheter not providing ongoing analgesia following the initial bolus. Block efficacy may also be limited in trials that examined only 1 type of TAP catheter placement (posterior or subcostal)15,18 against abdominal operations covering a range of dermatomes, some of which may be considered to fall outside the expected coverage of the TAP blockade (potentially showing analgesic inferiority due to inappropriate patient selection instead of
block success).
Future research will benefit from more structured categorization and standardization of thevariables that comprise a TAP catheter technique (insertion site, catheter type, initial blockade, infusate type, infusion regimen, and specific surgical intervention). Viewing these blocks as a composite technique as opposed to the binary means of how single-shot regional blocks are often viewed will help further define and refine the efficacy and applicability of TAP catheters, as well as assist in the framework for assessing other catheter plane blocks.
1. Schug S, Palmer G, Scott D, Halliwell R. Acute Pain Management:
Scientific Evidence. APMSE Working Group of the Australian and
New Zealand College of Anaesthetists and Faculty of Pain Medicine.
4th ed. Melbourne, Victoria, Australia: ANZCA & FPM; 2015.
2. Rodgers A, Walker N, Schug S,et al. Reduction of postoperative mortality
and morbidity with epidural or spinal anaesthesia: results from overview
of randomised trials. BMJ. 2000;321:1493.
3. Pöpping DM, Elia N, Van Aken HK, et al. Impact of epidural analgesia
on mortality and morbidity after surgery: systematic review and
meta-analysis of randomized controlled trials. Ann Surg. 2014;259:
1056–1067.
4. Lissauer J, Mancuso K, Merritt C, Prabhakar A, Kaye AD, Urman RD.
Evolution of the transversus abdominis plane block and its role in
postoperative analgesia. Best Pract Res Clin Anaesthesiol. 2014;28:
117–126.
5. Lee T, Barrington M, Tran T, Wong D, Hebbard P. Comparison of extent
of sensory block following posterior and subcostal approaches to
ultrasound-guided transversus abdominis plane block. Anaesth Intensive
Care. 2010;38:452–460.
6. Bujedo BM, Santos SG, Azpiazu AU. A reviewof epidural and intrathecal
opioids used in the management of postoperative pain. JOpioidManag.
2012;8:177–192.
7. Charlton S, Cyna AM, Middleton P, Griffiths JD. Perioperative
transversus abdominis plane (TAP) blocks for analgesia after abdominal
surgery [review]. Cochrane Database Syst Rev. 2010:CD007705.
8. Brogi E, Kazan R, Cyr S, Giunta F, Hemmerling TM. Transversus
abdominal plane block for postoperative analgesia: a systematic review
and meta-analysis of randomized-controlled trials. Can J Anaesth.
2016;63:1184–1196.
9. Gan TJ, Szafran M, Abrahams E. Update on emerging regional techniques
and novel local anesthetics in ambulatory anesthesia. Ambul Anesth.
2015;3:1–12.
10. Niraj G, Kelkar A, Hart E, et al. Comparison of analgesic efficacy of
four-quadrant transversus abdominis plane (TAP) block and continuous
posterior TAP analgesia with epidural analgesia in patients undergoing
laparoscopic colorectal surgery: an open-label, randomised, non-inferiority
trial. Anaesthesia. 2014;69:348–355.
11. Sanderson B, Doane M. Transversus abdominis plane catheters for
analgesia following abdominal surgery in adults. PROSPERO International
12
prospective register of systematic reviews. 2016:CRD42016037991.
Available at: http://www.crd.york.ac.uk/PROSPERO/display_record.asp?
ID=CRD42016037991. Accessed April 21, 2016.
12. MoherD,LiberatiA,TetzlaffJ, AltmanDG,GroupTP.PreferredReporting
Items for Systematic Reviews and Meta-analyses: the PRISMA
statement. PLoS Med. 2009;6:e1000097.
13. Abdallah FW, Chan VW, Brull R. Transversus abdominis plane block: a
systematic review. Reg Anesth Pain Med. 2012;37:193–209.
14. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD. The
Cochrane Collaboration’s tool for assessing risk of bias in randomised
trials. BMJ. 2011;343:d5928.
15. Wahba SS, Kamal SM. Analgesic efficacy and outcome of
transversus-abdominis plane block versus low thoracic-epidural analgesia
after laparotomy in ischemic heart disease patients. J Anesth. 2014;28:
517–523.
16. Ganapathy S, Sondekoppam RV, Terlecki M, Brookes J, Das Adhikary S,
Subramanian L. Comparison of efficacy and safety of lateral-to-medial
continuous transversus abdominis plane block with thoracic epidural
analgesia in patients undergoing abdominal surgery: a randomised,
open-label feasibility study. Eur J Anaesthesiol. 2015;32:797–804.
17. Heil JW, Nakanote KA, Madison SJ, et al. Continuous transversus
abdominis plane (TAP) blocks for postoperative pain control after hernia
surgery: a randomized, triple-masked, placebo-controlled study. Pain Med.
2014;15:1957–1964.
18. Rao Kadam V, Van Wijk RM, Moran JL, Miller D. Epidural versus
continuous transversus abdominis plane catheter technique for
postoperative analgesia after abdominal surgery. Anaesth Intensive Care.
2013;41:476–481.
19. Parikh BK, Waghmare V, Shah VR, Modi P. The analgesic efficacy of
continuoustransversus abdominisplaneblockinrenal transplantrecipients.
J Anaesthesiol Clin Pharmacol. 2015;31:531–534.
20. Serag Eldin M, Mahmoud F, El Hassan R, Abdel Raouf M, Afifi MH,
Yassen K. Intravenous patient-controlled fentanyl with and without
transversus abdominis plane block in cirrhotic patients post liver resection.
Local Reg Anesth. 2014;7:27–37.
21. Niraj G, Kelkar A, Jeyapalan I, et al. Comparison of analgesic efficacy of
subcostal transversus abdominis plane blocks with epidural analgesia
following upper abdominal surgery. Anaesthesia. 2011;66:465–471.
22. Zhong T, Ojha M, Bagher S, et al. Transversus abdominis plane block
reduces morphine consumption in the early postoperative period following
microsurgical abdominal tissue breast reconstruction: a double-blind,
placebo-controlled, randomized trial. Plast Reconstr Surg. 2014;134:
870–878.
23. Omar AM. Postoperative continuous transversus abdominis plane block vs
continuous woundinfusionof levobupivacaine infemales undergoing open
gynecologic procedures. Egypt J Anaesth. 2013;29:383–388.
24. Tammam T. Transversus abdominis plane block: the analgesic
efficacy of a new block catheter insertion method. Egypt J Anaesth.
2014;30:39–45.
25. Yoshida T, Furutani K, Watanabe Y, Ohashi N, Baba H. Analgesic efficacy
of bilateral continuous transversus abdominis plane blocks using anoblique
subcostal approach in patients undergoing laparotomy for gynaecological
cancer: a prospective, randomized, triple-blind, placebo-controlled study.
Br JAnaesth. 2016;117:812–820.
26. Maeda A, Shibata SC, Kamibayashi T, Fujino Y. Continuous subcostal
oblique transversus abdominis plane block provides more effective
analgesia than single-shot block after gynaecological laparotomy: a
randomised controlled trial. Eur J Anaesthesiol. 2015;32:514–515.
27. Børglum J, Jensen K, Christensen AF, et al. Distribution patterns,
dermatomal anesthesia, and ropivacaine serum concentrations after
bilateral dual transversus abdominis plane block. Reg Anesth Pain Med.
2012;37:294–301.
©2017 American Society of Regional Anesthesia and Pain Medicine
Copyright © 2017 American Society of Regional Anesthesia and Pain Medicine. Unauthorized reproduction of this article is prohibited.
Regional Anesthesia and Pain Medicine • Volume 43, Number 1, January 2018
TAP Catheters for Analgesia
28. Carney J, Finnerty O, Rauf J, Bergin D, Laffey JG, McDonnell JG. Studies
on the spread of local anaesthetic solution in transversus abdominis
plane blocks. Anaesthesia. 2011;66:1023–1030.
29. Finnerty O, McDonnellJG. Transversus abdominis plane block. CurrOpin
Anaesthesiol. 2012;25:610–614.
30. Khatibi B, Said ET, Sztain JF, et al. Continuous transversus abdominis
plane nerve blocks: does varying local anesthetic delivery
method—automatic repeated bolus versus continuous basal
infusion—influence the extent of sensation to cold?: A randomized,
triple-masked, crossover study in volunteers. Anesth Analg.2017;124:
1298–1303.
31. Hessian EC, Evans BE, Woods JA, Taylor DJ, Kinkel E, Bjorksten AR.
Plasma ropivacaine concentrations during bilateral transversus abdominis
plane infusions. Br J Anaesth. 2013;111:488–495.
32. Neal JM, Barrington MJ, Brull R, et al. The second ASRA practice
advisory on neurologic complications associated with regional anesthesia
and pain medicine: executive summary 2015. RegAnesthPainMed.2015;
40:401–430.
