Background and Objectives: The popliteal nerve plexus contributes to afferent knee-pain conduction. It is mainly formed by genicular branches from the posterior obturator and the tibial nerves, innervating the intra articular and posterior knee region. A subinguinal obturator nerve block al leviates pain after total knee arthroplasty. Reduced hip adductor motor function could be avoided by a posterior obturator nerve block inside the popliteal fossa.
The aim of this study was to evaluate the spread of dye after a distal ad ductor canal (AC) injection to the popliteal fossa and coloring of the pop liteal plexus and the genicular branch of the posterior obturator nerve by dissection. We also assessed the spread of dye into the popliteal fossa after a distal femoral triangle injection.
Methods: Tenmilliliters of dye was injected into the distal part of the AC in 10 cadaver sides andinto the distal part of the femoral triangle in 3 sides. Dissection was used to assess the spread of the injectate and coloring of the popliteal plexus and the genicular branch of the posterior obturator nerve, was well as the saphenous and medial vastus nerves.
Results: The popliteal plexus and the genicular branch of the posterior obturator nerve were dyed in all 10 dissections after AC injections. No dye spread into the popliteal fossa after femoral triangle injections.
Conclusions: Injection of 10 mL of dye into the distal part of the AC spreads into the popliteal fossa and colors the popliteal plexus and the genicular branch of the posterior obturator nerve.
(Reg Anesth Pain Med 2017;42: 725–730)
When aiming at alleviating severe pain after total knee arthroplasty (TKA) with peripheral nerve blocks, the challenge is to provide efficient analgesia while simultaneously pre serving the ability to ambulate early after surgery.1,2 A femoral triangle block generates anesthesia of the saphenous nerve, the
medial vastus nerve, and the medial femoral cutaneous nerve,3,4 alleviating pain from the anteromedial region of the knee5–7 without clinically affecting the ability to ambulate or increasing the risk of fall.8,9 The obturator nerve block has been demonstrated to play an important role in alleviating pain after TKA.3 The popliteal plexus is mainly formed by the genicular branches of the tibial and posterior obturator nerves, entwining the popliteal artery, and vein within the popliteal fossa.5,6 The terminal branches from the popliteal plexus reach the posterior capsule and innervate the posterior part and the intra-articular
structures of the knee joint.5 Paralysis of the hip adductor muscles could be avoided by blocking the posterior branch of the obturator nerve inside the popliteal fossa instead of blocking the obturator nerve inside the subinguinal region.
We hypothesized that an injection into the distal part of the adductor canal (AC) would spread alongside the femoral artery and vein through the adductor hiatus and into the popliteal fossa, thereby reaching the popliteal plexus and the genicular branch of the posterior obturator nerve.
The primary aims of the study were to assess the spread of the injectate from the distal end of the AC into the popliteal fossa on acadaver model and to assess if the posterior branch of the ob turator nerve and the popliteal plexus were reached by the dye. The secondary aims of the study were to evaluate the possible spread of the injectate from the AC proximally into the femoral tri angle and to assess if the saphenous and medial vastus nerves were dyed. Furthermore, we aimed to assess whether the dye injected into the femoral triangle at the midthigh level (midpoint between the base of the patella and anterior superior iliac spine [ASIS]) would spread throughout the AC and into the popliteal fossa to
dye the popliteal plexus and the genicular branch of the posterior obturator nerve.
Seven cadavers were donated to the Division of Clinical and Functional Anatomy of the Medical University of Innsbruck by men and women who had given their written informed con sent premortem to use their bodies after death for scientific and
educational purposes.
Ultrasound-guided injections of methylene blue were carried out bilaterally in the 7 cadavers (4 females and 3 males) except in 1 cadaver side that was not usable for ultrasound-guided injection (ie, 14 sides altogether). Ten cadaver sideshad aninjection into the AC, and 3 had an injection into the femoral triangle. Preservation
of the cadavers was carried out by arterial injection of an ethanol glycerol solution followed by 1 to 3 months of immersion in phenolic acid in water.10,11 The ultrasound-guided injections were performed using a high-frequency 15-6 MHz linear array probe
(X-Porte, Fujifilm; Sonosite, Inc, Bothell, Washington).
All the injections were performed by one of the authors (T.F.B.). Another author (B.M.), who was not present during the injection procedure, carried out all the dissections immediately after injection and documented the spread of dye.
Injection Procedure
With the cadaver positioned supine, the distance from the base of the patella to the ASIS was measured, and the midpoint was marked as the midthigh.
The apex of the femoral triangle was identified ultrasono graphically as the intersection of the medial borders of the sartorius and adductor longus muscles.4,7,12,13 This apex is an accurate proxy marker of the proximal end of the AC.7,14 The distance from this point to the ASIS and the midthigh was measured. The distal end of the AC was identified ultrasonographically as the passage of the femoral artery and vein through the adductor hiatus.
Adductor Canal Injections
The point of injection was approximately 1 to 2 cm proximal to the adductor hiatus. In 10 cadaver sides, an 80-mm, 22-gauge Stimuplex needle (B.Braun, Melsungen, Germany) was inserted in-plane, and 10 mL of methylene blue (2%) was injected into the AC, anteromedial to the femoral artery and vein.
Femoral Triangle Injections
The injections were carried out in 3 cadaver sides in the supine position. The point of injection was anterolateral to the femoral artery 2 to 3 cm proximal to the apex of the femoral triangle determined ultrasonographically, and the needle was inserted in-plane. Five milliliters of methylene blue (2%) was injected in 1 cadaver side, and 10 mL was injected on 2 cadaver sides. Relevant anatomical details are explained in more detail
in Figure 1.
Dissection Procedure
Subsequent to the injections, the cadavers were turned prone. The popliteal fossa was dissected, and the spread of dye into the popliteal fossawas assessed. Successful spread of dye was defined as coloring of the popliteal plexus, entwining the popliteal artery and vein, and the posterior branch obturator nerve. The cadaver
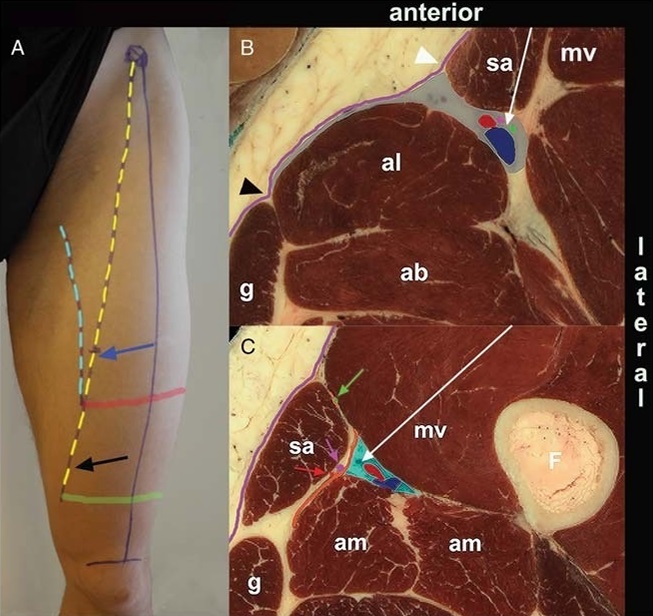
FIGURE 1. A,The needlein sertion points of the femoral triangle block (blue arrow) and the popliteal plexus block (black arrow). The cyan line indicates the medial border of the adductor longus, and the yellow line the medial border of the sartorius. These 2 lines delimit the femoral triangle (FT). The apex of the FT is indicated by the red stripe and the level of the adductor hiatus by the green stripe. Reproduced with permission from Wong et al14 (2017). B, Cross section of the FT (gray area) in the midthigh at the level of the blue arrow in A. The FT is delimited by the medial border (white arrowhead) of sartorius(sa), the medial border (black arrowhead) of adductorlongus (al), and roofedby
the fascia lata (magentastripe). The FT is a groove in the anterio rthigh, containing the femoral artery and vein (red and blue profiles in B and C), as well as the femoral nerve branches including the saphenous nerve (magenta dot) and medial vastus nerve (green dot). The FT block is performed by inserting the block needle (blue arrow in A and white arrow in B) in the midthigh with injection adjacent and lateral to the femoral artery and vein between the sartorius and medialvastus muscles. C, Cross sectionofthe distal part of the AC(cyan area) at the level of the black arrow in A. At this level, the femoral vessels dive deeper into the AC between the medial vastus (mv) anteriorly and the adductor magnus(am)posteriorly and away from the VAM (orangestripe) which is the anteromedialro of the AC.In this partof the AC, the saphenous nerve (magenta arrow) has pierced the VAM together with the descending geniculate artery (red arrow), entering the subsartorial compartment between the sartorius muscle and the VAM. The medial vastus nerve (green arrow) runs in its own fascial tunnel. ab indicates adductor brevis; F, femur; g, gracilis. Modified excerpt from VH Dissector with permission from Touch of Life Technologies Inc (www.toltech.net). Built on real anatomy from the National Library of Medicine’s Visible Human Project.
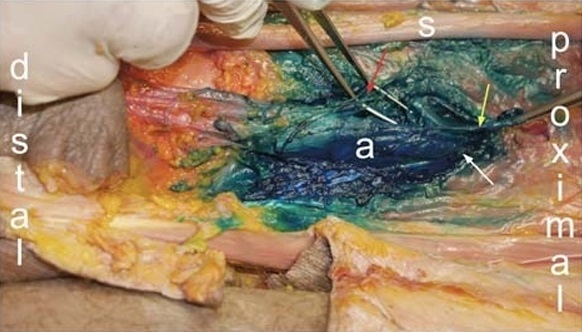
FIGURE 2. Spread of methylene blue from the AC through the adductorhiatus into the popliteal fossa. Sciatic nerve (S), popliteal vessels (a), popliteal plexus (red arrow), genicular ramus of the posterior obturator nerve (yellow arrow), adductor hiatus
(white arrow).
was then turned supine, and the AC and the femoral triangle were dissected. The proximal spread of injectate from the AC into the femoral triangle and coloring of the saphenous and the medial vastus nerves were assessed.
Posterior Dissection
Two initial transverse incisions were made to delineate the proximal-to-distal extension of the popliteal fossa. A second longitudinal incision combined the transverse incisions on their fibular side. The incisions cut through all superficial tissue layers, including the strong popliteal fascia. The thick tissue flap was raised and reflected medially to expose the muscular boundaries of the posterior genicular region: the semimembranosus muscle proximal-medial, the biceps femoris muscle proximal-lateral, and the medial and lateral heads of gastrocnemius muscle distally. If necessary, the incisions were extended. The popliteal fat pad was opened superficially and laterally by blunt dissection to free the main nerves, respecting the well-known variability of the location of the bifurcation the sciatic nerve. Subsequently, the entire fat pad was removed with great caution down to the common vascular she ath of the popliteal vessels. All the branches of the popliteal vessels and the entwining popliteal plexus nerve branches were spared and followed in order to distinguish innervation of muscles and joint capsule (Fig. 2). The semimembranosus muscle was retracted medially whereby the adductor hiatus was exposed be tween the 2 tendinous insertions of the adductor magnus muscle.
The terminal genicular branch of the obturator nerve was searched for and identified in the vicinity of the adductor hiatus (Figs. 2, 3A). Finally, the spread of dye was documented by opening the vascular sheath with complete exposure of the popliteal nerve plexus and its contributors (Fig. 2). The posterior branch of the obturator nerve was traced proximally to its exit from the obturator canal deep to the pectineus muscle in order to confirm the identity of the posterior obturator nerve.
Anterior Dissection
Two incisions were performed.The first followed the anterior surface of sartorius muscle from the ASIS distally to the level of the base of the patella. The second extended from the ASIS to the anterior margin of the gracilis muscle close to its origin. The tissue flap was raised and reflected medially. The sartorius muscle was lifted out of its fascial bed and transected at the midthigh level, and the remaining part of the fascia lata was removed. The distinct proximal rim of the vastoadductor membrane (VAM) was identified, and the neurovascular bundle (femoral artery, femoral vein, and saphenous nerve), entering the AC, was mobilized and separated from the nerve to the vastus medialis muscle (Fig. 4). The previously mentioned structures were followed
upward within the femoral triangle, and the saphenous nerve was exposed in its entire trajectory proximal to the VAM. Finally, the AC was opened by cutting through the VAM longitudinally in order to identify the structures contained inside the AC and to assess the spread of dye within the AC.
Ultrasonographic identification of the apex of the femoral triangle and the entire course of the femoral artery and vein throughout the femoral triangle and the AC was feasible in all 13 investigated cadaver sides. One of the 14 cadaver sides was physically disintegrated and excluded from the study prior to injection of the dye. Tencadaver sides had injections into the distal part of the AC (Fig. 1, A and C). The spread of dye extended into the popliteal fossa in 10 (100%) of 10 dissections (Fig. 2). The popliteal plexus was identified and colored as it entwined the popliteal artery
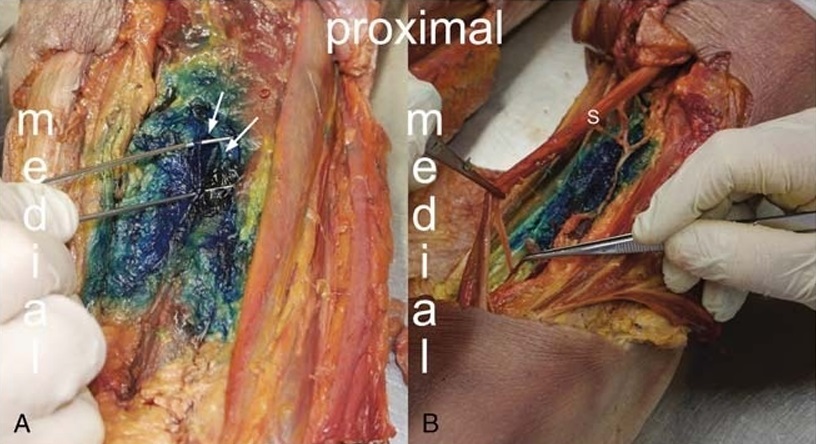
FIGURE 3. Coloring of nerve branches inside the popliteal fossa. A, Coloring of the genicular branch of the posterior obturator nerve (lifted by the forceps). B, The sciatic nerve (s) is not colored inside the popliteal fossa.
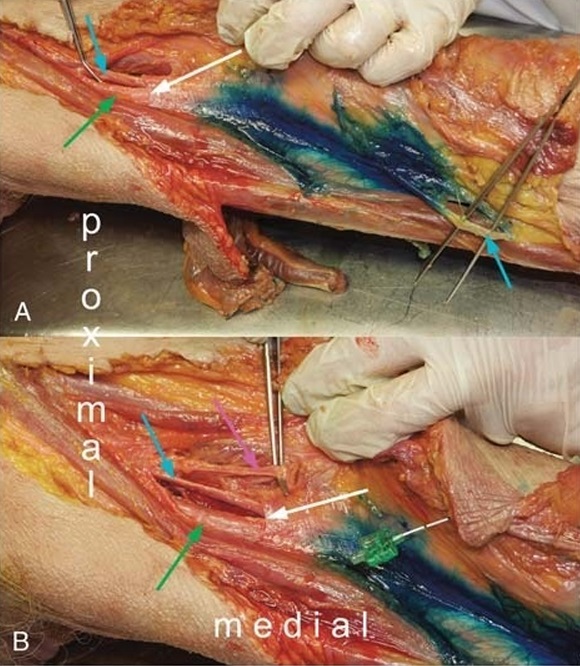
FIGURE 4. Proximal spread of methylene blue after injection into the AC. A, The saphenous nerve (cyan arrow) is the only nerve consistently found inside the AC, and it exits the AC by piercing the distal part of the VAM. Femoral artery (green arrow). B, The
medial vastus nerve (magenta arrow) is adjacent to the saphenous nerve inside the femoral triangle. The nerve to medial vastus deviates away from the saphenous nerve just proximal to the proximal entrance of the AC (whitearrow),where it enters its own fascial tunnel outside the AC.
and vein, distal to the adductor hiatus in all 10 sides (100%) (Fig. 2). The genicular branch from the posterior obturator nerve to the popliteal plexus was dyed inside the popliteal fossa in all 10 sides (100%) (Figs. 2 and 3). The entrance of the terminal
branch of the posterior obturator nerve into the popliteal fossa varied: from the posterior surface of the adductor magnus muscle in 3 (30%) of 10 sides, from the margin of the adductor hiatus in 2 (20%) of 10 sides, and through the distal 1 cm of the AC in 5
(50%) of 10 sides. The sciatic nerve was stained in 1 (10%) of 10 sides, and the tibial genicular branches distal to the popliteal plexus were colored in 2 (20%) of 10 sides (Figs. 1F, 3B). In 1 cadaver side, a ramus from the tibial nerve branched off in the
distal part of the popliteal fossa and reversed along the popliteal artery to reach the popliteal plexus in the proximal part of the popliteal fossa.
Dye injected into the AC stained the saphenous nerve in all cadaver sides (100%) before the nerve pierced the distal part of the VAM (Fig. 4). Proximal spread from the AC into the femoral triangle was observed in 4 sides (40%) and colored the medial
vastus nerve inside the femoral trianglein3 sides (30%). In 7 sides (70%), the proximal spread did not dye the medial vastus nerve (Figs. 1, 4). Injection of methylene blue into the femoral triangle proxi malto the ultra sono graphically identified entrance of the AC dyed both the saphenous nerve and the medial vastus nerve inside the femoral triangle in 3 (100%) of 3 dissected sides (Fig. 5A).
The injectate did spread distally from the femoral triangle into the AC in all 3 cadaver sides but did not spread throughout the adductor hiatus into the popliteal fossa in any of the 3 cadaver sides (Fig. 5B). The injectate did spread proximally in the femoral triangle as far as 2, 4 cm (the 5-mL injectate) and 8 cm from the inguinal crease (Fig. 1A).
The medial vastus nerve was identified inside the femoral triangle and descended inside its own fascial tunnel anterior and superficial to the VAM in all 13 sides (100%) (Fig. 4).
The saphenous nerve was the only nerve identified inside the ACin all 13 cadaver sides (100%) (Figs. 1C, 4). The apex of the femoral triangle was identified ultrasono graphically in all 13 cadaver sides (100%) (Fig. 1C). The midpoint of the thigh gauged as midway between the base of the patella and the ASIS was located proximal to the apex of the femoral triangle identified ultra sono graphically in all 13 sides (100%) (Fig. 1B).
In the present cadaver study, we identified the genicular branch of the posterior obturator nerve and the popliteal plexus inside the popliteal fossa distal to the adductor hiatus as described by Gardner5 in 1948. We demonstrated a spread of injectate into
the popliteal fossa after injecting 10 mL of dye into the AC near the adductor hiatus. The popliteal plexus and the genicular branch of the posterior obturator nerve were stained consistently inside the popliteal fossa. Several studies have reported a spread of injectate to the popliteal fossa after injection into the AC, but none of these studies have assessed whether the injectate reached the popliteal plexus and the genicular branch of the posterior obturator nerve.15–18 The latter plays an important clinical role in knee
pain after TKA.3,19,20 The obturator nerve can be anesthetized by an ultrasound-guided subpectineal injection of local anesthetic at the level of the inguinal crease.21 The subpectineal obturator nerve block approach produces paralysis of a major part of the
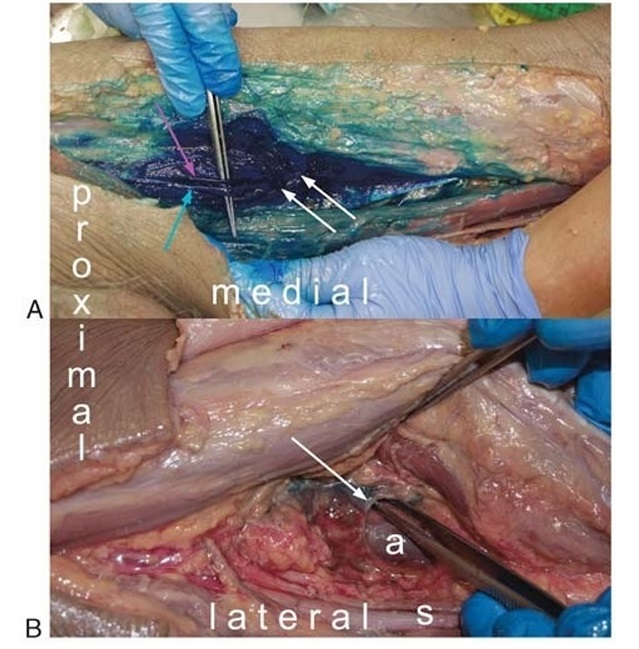
FIGURE 5. A, Apex of femoral triangle. The spread of methylene blue injected into the femoral triangle, coloring the saphenous nerve (cyan arrow) and the medial vastus nerve (magenta arrow). The white arrows indicate the proximal entrance of the AC.
B, Popliteal fossa. Methylene blue injected into the femoral triangle does not enter the popliteal fossa. The white arrow indicates the adductor hiatus, that is, the distal end of the AC. Popliteal artery (a), sciatic nerve (s).
hip adductor muscles.3,19,20 Our results in the present study sug gest that an injection of 10 mL of local anesthetic into the distalpart of the AC could anesthetize the genicular branch of the posterior obturator nerve in the popliteal fossa. Postoperative ambula
tion might be improved by the popliteal plexus block via the AC compared with the subpectineal obturator nerve block in the subinguinal region.3,21 In addition, anesthesia of the tibial genicular nerve branches of the popliteal plexus with the AC approach might
improve analgesia compared with a subpectineal obturator nerve block after TKA. Goffin et al18 reported spread of injectate into the popliteal fossa after injection of 20-mL dye into the AC and observed staining of the sciatic nerve in all cases, but staining of the popliteal vessels in only 3 of 8 cadavers. The results of Goffin et al18 do not agree with our present study. Injection of 10 mL of dye into the AC did spread consistently via the adductor hiatus into the popliteal fossa and always stained the popliteal vessels.
Furthermore, the sciatic nerve was stained in only 1 of 10 cases probably because of injection of a lower volume (10 mL) com pared with Goffin et al.18 It can be speculated that an injection of a larger volumewould increase the risk of anesthesia of the sciatic nerve with an associated increased risk of fall and reduction of the ability to ambulate.16 Furthermore, the analgesic effect of a sciatic block after TKA is not even clinically convincing.22,23
The saphenous nerve was the only nerve consistently found inside the AC, and it always pierced the distal part of the VAM to enter the subsartorial compartment. Contrary to a recent ca daver study, we consistently located the medial vastus nerve in all cadaver sides inside its own fascial tunnel and definitely out side the AC.24 The midpoint of the thigh was proximal to the AC inall cadaver sides, similar to the findings by Bendtsen et al7 and Wong et al.14 Several studies have made the claim that the midpoint of the thigh—defined as the midpoint between the ASIS and the base of the patella—is within the AC.8,9,25–34 Thus, studies comparing the analgesic efficiency of a femoral triangle block with a nerve block techniquewhere the local anesthetic is injected into the AC proper should be interesting for future research. Further studies are also warranted to determine the extent of spread of different local anesthetic volumes injected into the distal end of the AC, as well as the clinical effect of local anesthetic
injected into the popliteal fossa. In conclusion, this study demonstrates that dye injected into the distal end of the AC spreads into the popliteal fossa and stains the popliteal plexus and the genicular branch of the posterior obturator nerve in cadavers. Injection of dye into the femoral triangle does not spread into the popliteal fossa. The saphenous nerve was the only nerve consistently found inside the AC. The medial vastus nerve descended inside its own fascial tunnel outside the ACin all cadavers.
The authors thank the individuals who donated their bodies and tissues for the advancement of education and research.
1. Holm B, Kristensen MT, Myhrmann L, et al. The role of pain for early
rehabilitation in fast track total knee arthroplasty. Disabil Rehabil.
2010;32:300–306.
2. Kehlet H, Thienpont E. Fast-track knee arthroplasty—status and future
challenges. Knee. 2013;20(suppl 1):S29–S33.
3. Runge C, Børglum J, Jensen JM, et al. The analgesic effect of obturator
nerve block added to a femoral triangle block after total knee arthroplasty:
a randomized controlled trial. Reg Anesth Pain Med.2016;41:
445–451.
4. Bendtsen TF, Moriggl B, Chan V, Borglum J. Basic topography of the
saphenous nerve in the femoral triangle and the adductor canal. Reg Anesth
Pain Med. 2015;40:391–392.
5. GardnerE.Theinnervationofthekneejoint.AnatRec. 1948;101:109–130.
6. HornerG,DellonAL.Innervationofthehumankneejointandimplications
for surgery. Clin Orthop Relat Res.1994:221–226.
7. Bendtsen TF, Moriggl B, Chan V, Børglum J. The optimal analgesic block
for total knee arthroplasty. RegAnesthPainMed. 2016;41:711–719.
8. Grevstad U, Jaeger P, Sorensen JK, et al. The effect of local anesthetic
volumewithin the adductor canal onquadriceps femoris function evaluated
by electromyography: a randomized, observer- and subject-blinded,
placebo-controlled study in volunteers. Anesth Analg. 2016;123:493–500.
9. Sorensen JK, Jaeger P, Dahl JB, Gottschau B, Stephensen SL, Grevstad U.
The isolated effect of adductor canal block on quadriceps femoris muscle
strength after total knee arthroplasty: a triple-blinded, randomized,
placebo-controlled trial with individual patient analysis. Anesth Analg.
2016;122:553–558.
10. Platzer W, Putz R, Poisel S. New system for the preservation and storage of
anatomical matter [in German]. Acta Anat (Basel). 1978;102:60–67.
11. Kessler J, Moriggl B, Grau T. Ultrasound-guided regional anesthesia:
learning with an optimized cadaver model. Surg Radiol Anat.2014;36:
383–392.
12. BendtsenTF, MorigglB, ChanV,Pedersen EM, BørglumJ. Redefining the
adductor canal block. RegAnesthPainMed.2014;39:442–443.
13. Bendtsen TF, Moriggl B, Chan V, Pedersen EM, Børglum J. Defining
adductor canal block. RegAnesthPainMed.2014;39:253–254.
14. Wong WY, Bjørn S, Strid JM, Børglum J, Bendtsen TF. Defining the
location of the adductor canal using ultrasound. Reg Anesth Pain Med.
2017;42:241–245.
15. Andersen HL, Andersen SL, Tranum-Jensen J. The spread of injectate
during saphenous nerve block at the adductor canal: a cadaver study. Acta
Anaesthesiol Scand. 2015;59:238–245.
16. Gautier PE, Hadzic A, Lecoq JP, Brichant JF, Kuroda MM, Vandepitte C.
Distribution of injectate and sensory-motor blockade after adductor canal
block. Anesth Analg. 2016;122:279–282.
17. Jaeger P, JenstrupMT,LundJ,etal.Optimal volumeoflocalanaesthetic for
adductor canal block: using the continual reassessment method to estimate
ED95. Br J Anaesth. 2015;115:920–926.
18. Goffin P, Lecoq JP, Ninane V, et al. Interfascial spread of injectate after
adductor canal injection in fresh human cadavers. Anesth Analg. 2016;123:
501–503.
19. McNamee DA, Parks L, Milligan KR. Post-operative analgesia following
total knee replacement: an evaluation of the addition of an obturator nerve
block to combined femoral and sciatic nerve block. Acta Anaesthesiol
Scand.2002;46:95–99.
20. Macalou D, Trueck S, Meuret P, et al. Postoperative analgesia after total
knee replacement: the effect of an obturator nerve block added to the
femoral 3-in-1 nerve block. Anesth Analg. 2004;99:251–254.
21. Taha AM. Brief reports: ultrasound-guided obturator nerve block: a
proximal interfascial technique. Anesth Analg. 2012;114:236–239.
22. Abdallah FW, Chan VW, Gandhi R, Koshkin A, Abbas S, Brull R. The
analgesic effects of proximal, distal, or no sciatic nerve block on posterior
knee pain after total knee arthroplasty: a double-blind placebo-controlled
randomized trial. Anesthesiology. 2014;121:1302–1310.
23. Abdallah FW, Madjdpour C, Brull R. Is sciatic nerve block advantageous
when combined with femoral nerve block for postoperative analgesia
following total knee arthroplasty? A meta-analysis. Can J Anaesth.2016;
63:552–568.
24. Burckett-St Laurant D, Peng P, Giron Arango L, et al. The nerves of the
adductor canal and the innervation of the knee: an anatomic study.
RegAnesthPainMed.2016;41:321–327.
©2017 American Society of Regional Anesthesia and Pain Medicine 729
Copyright © 2017 American Society of Regional Anesthesia and Pain Medicine. Unauthorized reproduction of this article is prohibited.
Runge et al
Regional Anesthesia and Pain Medicine • Volume 42, Number 6, November-December 2017
25. Grevstad U, Mathiesen O, Lind T, Dahl JB. Effect of adductor canal block
on pain in patients with severe pain after total knee arthroplasty: a
randomized study with individual patient analysis. Br JAnaesth. 2014;112:
912–919.
26. Henningsen MH, Jaeger P, Hilsted KL, Dahl JB. Prevalence of saphenous
nerve injury after adductor-canal-blockade in patients receiving total knee
arthroplasty. Acta Anaesthesiol Scand. 2013;57:112–117.
27. Jaeger P, Grevstad U, Henningsen MH, Gottschau B, Mathiesen O, Dahl
JB. Effect of adductor-canal-blockade on established, severe post-operative
pain after total knee arthroplasty: a randomised study. Acta Anaesthesiol
Scand.2012;56:1013–1019.
28. Jæger P, Koscielniak-Nielsen ZJ, Schrøder HM, et al. Adductor canal
block for postoperative pain treatment after revision knee arthroplasty:
a blinded, randomized, placebo-controlled study. PLoS One.
2014;9:e111951.
29. Jenstrup MT, Jaeger P, Lund J, et al. Effects of adductor-canal-blockade on
pain and ambulation after total knee arthroplasty: a randomized study. Acta
Anaesthesiol Scand. 2012;56:357–364.
730
30. Jaeger P, Zaric D, FomsgaardJS, etal. Adductor canal blockversus femoral
nerve block for analgesia after total knee arthroplasty: a randomized,
double-blind study. RegAnesthPainMed. 2013;38:526–532.
31. Lund J, Jenstrup MT, Jaeger P, Sørensen AM, Dahl JB. Continuous
adductor-canal-blockade for adjuvant post-operative analgesia after major
knee surgery: preliminary results. Acta Anaesthesiol Scand.2011;55:
14–19.
32. Mudumbai SC, Kim TE, Howard SK, et al. Continuous adductor canal
blocks are superior to continuous femoral nerve blocks in promoting early
ambulation after TKA. Clin Orthop Relat Res. 2014;472:1377–1383.
33. Shah NA, Jain NP. Is continuous adductor canal block better than
continuous femoral nerve block after total knee arthroplasty? Effect on
ambulation ability, early functional recovery and pain control: a
randomized controlled trial. J Arthroplasty. 2014;29:2224–2229.
34. Shah NA, Jain NP, Panchal KA. Adductor canal blockade following total
knee arthroplasty-continuous or single shot technique? Role in
postoperative analgesia, ambulation ability and early functional recovery: a
randomized controlled trial. J Arthroplasty. 2015;30:1476–1481.
