Background and Objectives: The analgesic effect and duration of a transversus abdominis plane (TAP) block remain controversial. Transversus abdominis plane blocks are effective for somatic/incisional pain but do not provide analgesia for visceral pain from intra-abdominal procedures. The purpose of this study was to assess the area and extent of cutaneous sensory blockade and the regression of dermatomal anesthesia after bilateral oblique subcostal TAP block.
Methods: This observational, prospective clinical study consisted of 12 healthy volunteers. All volunteers received a bilateral oblique subcostal TAP block under real-time ultrasound guidance with 20 mL of 0.375% ropivacaine.Theanteriorabdominalcutaneousareawasdividedinto3parts (midabdomen, left-lateral abdomen, right-lateral abdomen) using 2 lines drawn in a parasagittal fashion 5 cm lateral to the midline. The area of cu taneous sensory blockade involving the anterior abdomen was assessed 30 minutes after institution of the block using a cold stimulus. This was followed by repeated measurements using a cold stimulus applied along parasagittal lines drawn 3 cm lateral to the midline at 0.5, 6, 10, 14, 18, 22, and 26 hours after blockade.
Results: The area of cutaneous sensory blockade of the abdomen was 332 (SD, 73) cm2; that of the midabdomen was 253 (SD, 29) cm2,which represented an average of 90% of the area of the midabdomen; and that of the lateral abdominal wall (combination of left-lateral abdomen and right-lateral abdomen) was 79 (SD, 62) cm2, which represented an average of 26% of total lateral abdominal area. Dermatomes T7–T12 of the midabdomen were successfully blocked in all volunteers after using the bilateral oblique subcostal technique. However, T6 and L1 were only variably blocked. The area of cutaneous sensory block of the anterior abdomen regressed over the ensuing 22 hours in the following manner: 90%, 87%, 73%, 50%, 22%, 3%, and 0% at 0.5, 6, 10, 14, 18, 22, and 26 hours, respectively.
Conclusions: Bilateral oblique subcostal TAP block produces a wide spread cutaneous sensory blockade with a consistent dermatomal distribution in the midabdomen for a considerable effective duration.
(Reg Anesth Pain Med 2018;43: 174–179)
Various major abdominal surgical procedures are associated with severe postoperative pain. Recently, there has been in creasing interest in using TAP blocks as a supplement to multi modal analgesia regimens for major abdominal surgeries.1–4 Rafi5 described the landmark-based triangle of Petit (transversus abdominis plane [TAP]) block in 2001, and the ultrasound-guided posterior TAP block was first advanced by Hebbard et al6 in 2007.
Arora et al7 reported that the TAP block reduced postoperative pain up to 24 hours after laparoscopic hernia repair. Previously, Tran et al8 had demonstrated that segmental nerves T10, T11, T12, and L1 of cadaveric specimens injected with dyewere involved in 50%, 100%, 100%, and 93% of cases, respectively
(by simulating the TAP block between costal margin and iliaccrest).However, in major gynecological cancer surgery, TAP blocks have not been shown to be effective in reducing morphine consumption and improving postoperative pain relief.9 This finding in gynecological surgery seems to be supported by the
recent work of Stoving et al10 that indicates TAP blocks result in a large variation in nondermatomal cutaneous sensory block distribution.
The oblique subcostal TAP block was described by Hebbard et al11 in2010.Shinetal12 reported that the oblique subcostal TAP block was an effective analgesic method for patients under going laparoscopic cholecystectomy. In addition, in 2013, we also reported that bilateral oblique subcostal TAP blocks were more ef fective than intravenous opioid analgesia for patients undergoing elective radical gastrectomy.13 To date, there are no detailed studies focusing on cutaneous sensory block distribution and its duration for the oblique subcostal TAP block.
Based on our previous study13 and clinical experiences, we hypothesized that a bilateral oblique subcostal TAP block could produce a widespread and consistent cutaneous sensory block in the midabdomen. Therefore, we performed the bilateral oblique subcostal TAP block in healthy volunteers in
order to calculate the area of cutaneous sensory blockade of the abdomen and to describe the temporal regression of the blocked dermatomes.
This study was approved by the ethics committee of the First Affiliated Hospital of Wenzhou Medical University. Written consent was obtained from all subjects. This trial was registered in the Chinese Clinical Trial Registry (ChiCTR-OOC-16009037). Twelve volunteers were recruited. Demographic data of volunteers were mean age, 42 (SD, 7) years; sex (female/male), 8/4; weight, 60 (SD, 9) kg; height, 1.6 (SD, 0.06) m; and body mass index 23 (SD, 5) kg/m2. Inclusion criteria were age older than 18 years and an abdomen with intact cutaneous sensation as demonstrated by testing with a cold stimulus. Exclusion criteria were history of allergy to ropivacaine or other drugs used in this trial, inability to communicate, American Society of Anesthesiologists classification
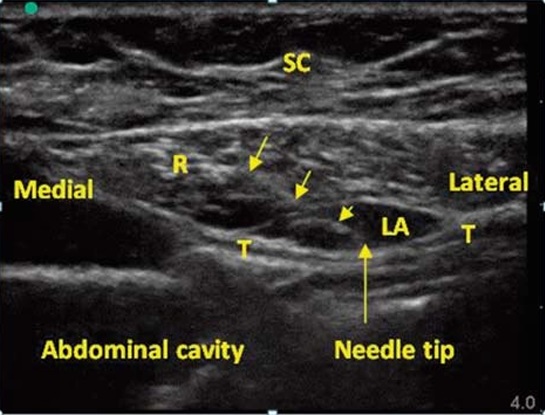
FIGURE 1. Sonograms of the anterior abdominal wall near the costal margin showing the continuity of the transversus abdominis (T) posterior to the rectus abdominis (R). The fascial plane was confirmed when a convex lens-shaped collection of local anesthetics (LA) was found between the rectus abdominis (R) sheath and the transverses abdominis (T). SC indicates subcutaneous tissue. Arrowheads points to needle used for anesthetic administration.
3 or greater, body mass index 18 kg/m2 or less or 30 kg/m2 or greater, spinal deformities, neuropathy, spinal cord disorders, an abdominal scar, and/or a history of abdominal surgery. Intravenous access was established after the subject was ad
mitted into the designated block ward, and routine monitoring was performed in all participants (noninvasive blood pressure, continuous electrocardiogram, and pulse oximetry) during the TAP block period and 60 minutes after complete neurosensory
resolution of the block.
All participants were kept in the supine position and sedated with a 1- to 2-mL intravenous mixture of 20 μg/mL fentanyl and 1 mg/m L midazolam. During the block, a 10-cm needle was used with an high frequency linear 38-mm 6- to 15-MHz linear trans
ducer (SonoSite X-Porte; SonoSite Inc, Bothell, Washington). The operator placed the ultrasound probe inferior and parallel to the costal margin and scanned along the oblique subcostal line. This scan/examination was from the xiphoid to the anterior
portion of the iliac crest in order to identify the 4 muscles of the anterior and lateral abdominal wall (rectus abdominis, external oblique, internal oblique, and transversus abdominis). Caudal to the costal margin and medial to the semilunaris, a portion of
the transversus abdominis usually extends beneath the rectus abdominis, near the xiphoid. The probe was tilted inferior medially to get a clear ultrasound image of the transversus abdominis muscle beneath the rectus abdominis muscle, thereby allowing a
closer approach to the xiphoid with the TAP block. Effective needle placement for the TAP block was achieved using an in plane technique near the xiphoid with subsequent injection of 1 to 2 mL of local anesthetic solution into the fascial plane to confirm the location of needle tip in the target plane. Proper needle positioning was confirmed when a convex lens-shaped collection of fluid was identified between the rectus abdominis
sheath and the transversus abdominis (Fig. 1). Local anesthetic was then injected incrementally to dilate the intermuscular space (hydrodissection). The dilating plane was opened anterior to the needle, and the needle was advanced toward the lateral-inferior end of the dilating plane (with simultaneous manipulation of needle advancement and hydrodissection). This sequence was repeated until the edge of the transducer reached the anterior part of the iliac crest. Using needle advancement and hydrodissection (starting near the xiphoid and costal margin), the needle was passed between rectus abdominis sheath and the transversus abdominis. It was then directed beneath the aponeurosis of the linea semilunaris and passed through the fascial layer of the in ternal abdominis and transversus abdominis muscles toward the anterior portion of the iliac crest. A6-to7-mLvolumeofsolution was required for the hydro dissection in the TAP medial to the semilunaris. The remainder of the volume was used to hydrodissect the planes between internal abdominis and transversus abdominis. Note that during the block procedure only local anesthetic was used for the hydrodissection, and this volume (used for hydrodissection) was the only volume
used/required for the TAP block; there was no additional local an esthetic administration. We used a 10-cm needle in our study, rather than the 15- to 20-cm needleused by Hebbard et al.11 In doing so, we ascertained that the needle must be retracted and reinserted into the plane repeatedly (4–5 times) along the oblique subcostal line to accomplish the TAP block successfully. The bi lateral oblique subcostal TAP block was performed with 20 mL of 0.375% ropivacaine (batch no. X980550; AstraZeneca, Cambridge, United Kingdom) administered along each side of the oblique subcostal line, thereby producing a zone of local anesthetic diffusion from the xiphoid to the anterior superior iliac spine.
Measurement and Calculation
The boundary of the anterior abdomen consists of the following surface landmarks: the xiphoid process, the costal margin, the
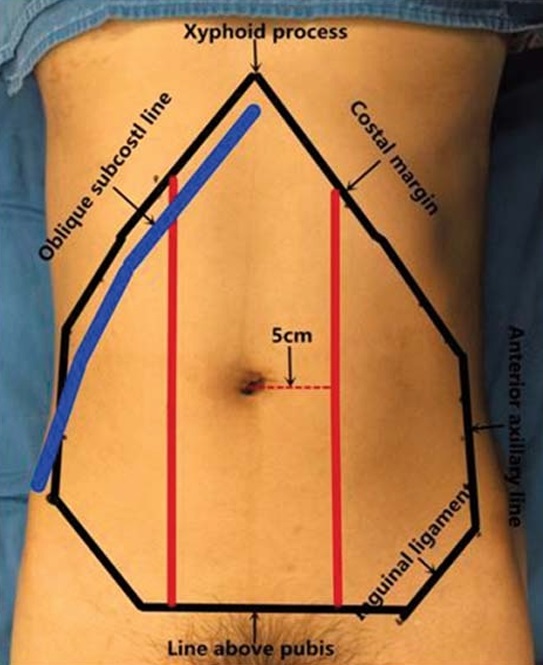
FIGURE 2. The black line outlines the cutaneous area of the anterior abdominalwall. The two parasagittal red lines 5 cmlateral to midline divide the anterior abdominal wall into three parts (mid-abdomen,left lateral-abdomen,right lateral-abdomen). The blue line represents the oblique subcostal line from the xyphoid process to the anterior part of iliac crest.
anterior axillary line, the iliac crest, the inguinal ligament, and the symphysis ossium pubis. The anterior abdominalwall was further divided into 3 portions: (1) midabdomen, (2) left-lateral abdomen, and (3) right-lateral abdomen, using 2 parasagittal lines 5 cm lateral to midline as shown in Figure 2.
The abdominal cutaneous sensory block area was tested (by 1 investigator) using a cold stimulus (ice cube) starting 30 minutes after the end of block administration. We used a dichotomous method (successful block/failed block) to assess the cutaneous
sensory changes (as identified by the application of the cold stimulus). We defined a block as successful when the sensation to cold was lost or markedly reduced, and a failed block when the sensation to cold was reduced (but still sensitive to cold), or the persistence of normal sensation. The cold stimulus was moved laterally at approximately 2 cm/s from midline at 1-cm intervals and stopped at the anterior axillary line. During application of the cold stimulus, areas of sensory change (from successful block to failed block) were marked on the skin, and the marked dots were connected to map the blocked area. A transparent rectangular device was applied to the abdomen to assist with mapping/identification of sensory changes. Thereafter, all surface landmarks/lines were transferred to it.
Atransparent digital-based image was achieved with a fixed pixel value (3456*4912) (insizeA3 [1217 cm2]) by scanning the transferred transparency using Bizhub Press c7000 (Konica Minolta Holdings, Inc., Marunouchi, Japan) and saved in JPG format. The digital image was opened using Adobe Photoshop CS (Adobe Systems, San Jose, California). We selected the targeted region by using a magnetic lasso tool. The pixel value of the selected region (PV-R) was calculated by the histogram application. The actual area of the digital image was 1217 cm2; this corresponded to the area of the targeted region on digital image (1217*[PV-R/fixed pixel value] cm2).14
The lines on the abdominalwallwere removed when the trans fer drawing was completed. The segmental dermatomes on both sides were marked using 2 parasagittal lines 3 cm lateral to midline, according to standard dermatome charting (the T6 dermatome at the level of the xiphoid process, T8 at the lower curve of costal margin, T10 at the umbilicus, T12 at the level just above symphysis ossium pubis, and L1 at the inguinal ligament). The marked derma tomes were repeatedly tested by the application of the cold stimulus at 0.5, 6, 10, 14, 18, 22, and 26 hours after blockade.
Statistical Analysis
Statistical analyses were performed using SPSS Statistics for Windows (version 17.0; SPSS Inc, Chicago, Illinois). Variables and demographics were presumed to follow a Gaussian distribution and are expressed as mean (SD), whereas other data are expressed as median and interquartile ranges).
The volunteers recruited into this study (n = 12) received a bilateral oblique subcostal TAP block under ultrasound guidance according to the study protocol. A volume of 20 mL of 0.375% ropivacaine was used for hydrodissection (and anesthesia) in the TAP along the oblique subcostal line from the xiphoid process to the anterior portion of iliac crest in the hemiabdomen of all volunteers.
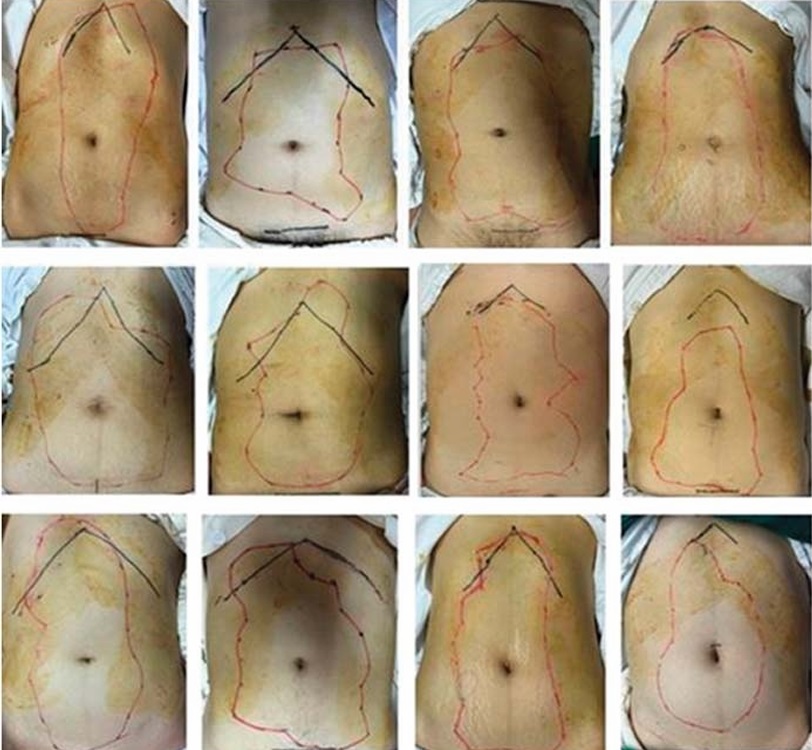
FIGURE 3. Photographs of cutaneous sensory block area 30 minutes after bilateral oblique subcostal TAP block on anterior abdominal wall of 12 volunteers. The red line outlines the blocked area on abdominal skin tested by cold stimulus.
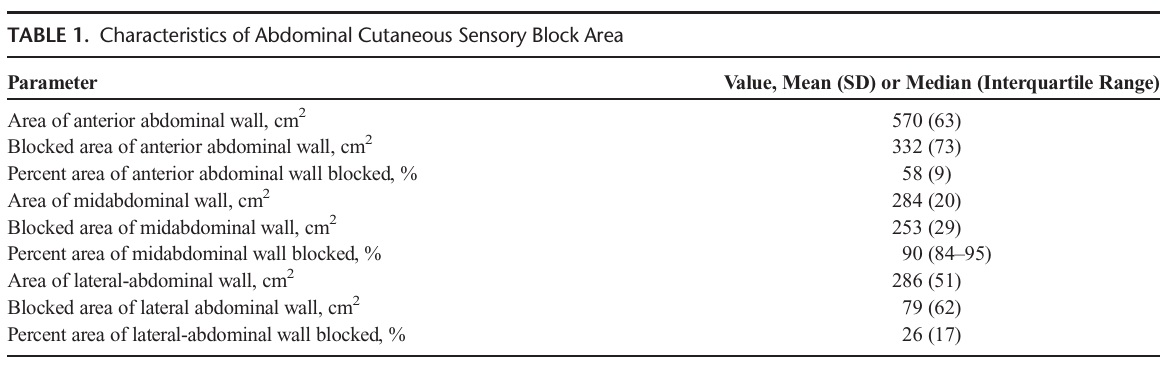
Thirty minutes following bilateral oblique subcostal TAP block, the cutaneous sensory block area was tested using a cold stimulus (ice cube) as depicted in Figure 3. The total blocked area of the abdomen at 30 minutes was estimated to be 332 (SD, 73) cm2. The blocked area of the midabdomen was 253 (SD, 29) cm2 (90% of the midabdomen skin was determined to have been successfully anesthetized). The total blocked area of the lateral ab dominal wall (combination of left-lateral abdomen and right lateral abdomen) was estimated to be 79 (SD, 62) cm2 equaling 26% of total lateral abdominal area (Table 1).
The percentage of blocked dermatomes (T7–T12) at 30 minutes was 100%.However,T 6 and L 1 had a lower percent age of success (Fig. 4).The blockade of the anterior abdomen regressed over the ensuing 26 hours: 90%, 87%, 73%, 50%, 22%, 3%, and 0% at 0.5, 6, 10, 14, 18, 22, and 26 hours, respectively (Fig. 5).
Our study demonstrated that a bilateral oblique subcostal TAP block with a low volume of local anesthetic produced a widespread consistent cutaneous sensory block in the anterior abdominal wall under real-time ultrasound guidance (90% of the midabdomen was successfully blocked, and the lateral ab dominal wall was successfully blocked to a lesser extent). The successful block rates of dermatomes T7 to T12 were 100%,
with T6 and L1 at 75% and 50%, respectively. The majority of segmental dermatomes (87%) had a 10-hour duration of blockade, and some dermatomes (3%) had evidence of block ade up to 22 hours.
Several clinical trials have shown that TAP blocks with vari ous approaches (lateral, subcostal, oblique subcostal) can success fully anesthetize the anterolateral abdominal wall to alleviate postoperative somatic pain and reduce opioid consumption after
abdominal and pelvic surgeries.1,2,13,15 However, Ghisi et al16 recently found that ultrasound-guided lateral TAP blocks were not effective in reducing postoperative morphine consumption in patients undergoing total laparoscopic hysterectomy. Another recent study has also shown that ultrasound-guided lateral TAP blocks cannot provide beneficial postoperative pain relief anda re duced opioid consumption after laparoscopic colorectal cancer surgery.17 Furthermore, a volunteer study by Stoving et al 10 demonstrated that single-injection lateral TAP blocks produced only
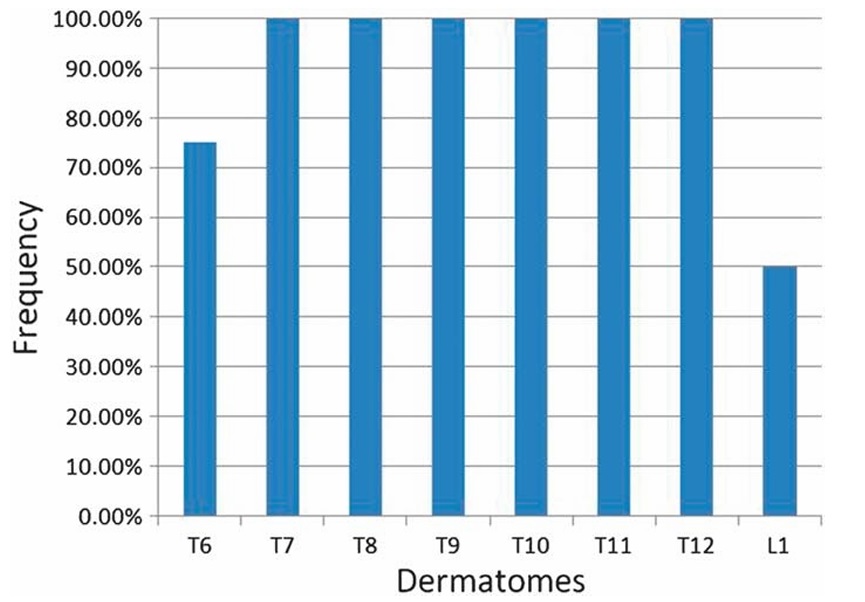
FIGURE 4. Frequency of dermatomes blocked at 30 minutes after completion of bilateral oblique subcostal TAP block tested along parasagittal lines 3 cm lateral to midline.
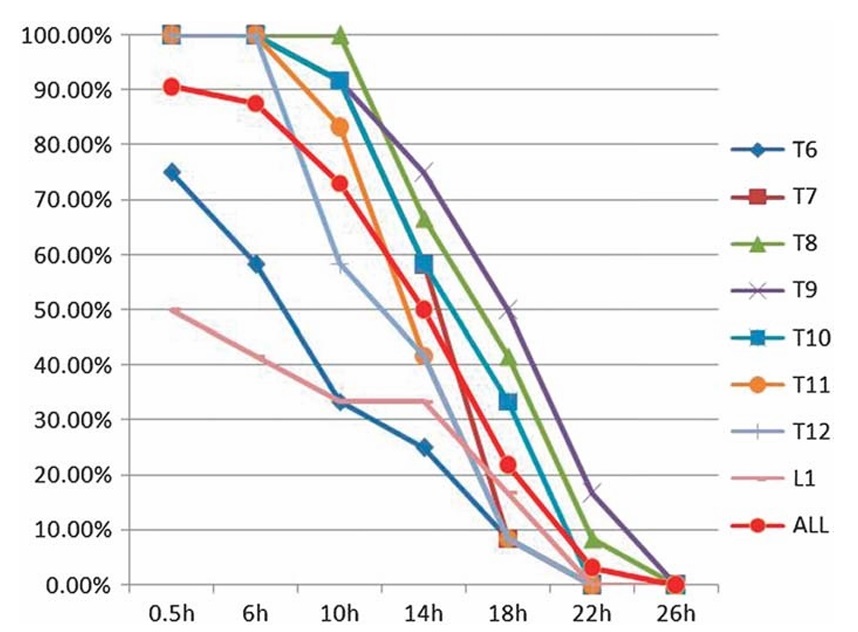
FIGURE 5. Regression of area blocked after bilateral oblique subcostal TAP block. The red curved line represent percentage of total blocked area fromT6to L 1 at different time points. The percentages of total blocked area of anterior abdomen are 90%, 73%,50%, 22%, 3%,and 0%, respectively, at 30 minutes, 10H, 14H, 18H, 22H, 26H after block.
small areas of effective cutaneous sensory anesthesia with large variations in the anterior abdominal wall. Nonetheless, the oblique subcostal TAP block has been demonstrated to be effective in reducing postoperative pain for abdominal surgery.12,18 In our previous work,13 we also found that the analgesic effect of an oblique subcostal TAP block performed before surgery was evi dent andeffective in the first 6 hours postoperatively after radical gastrectomy. The present study demonstrates that the area of successful cutaneous sensory blockade of the midabdomen (as determined by a cold stimulus) was 253 (SD, 29) cm2 (90% of the midabdomen was determined to have been successfully anesthetized).
In our study, directing the needle inferior laterally to progressively distend (hydrodissection) the transversus abdominis muscle plane was effective. We were able to infiltrate local anesthetic from the xiphoid to the anterior superior iliac spine under the
oblique subcostal line, thereby blocking the intercostal nerves as they emerge into the transversus plane. This allowed us to use a low volume of local anesthetic (40 mL) that was less than that used by Hebbard et al.11 Hebbard et al 11 had to inject an additional
10 to 15 mL of local anesthetic at the superior and inferior limits of the hydrodissection on the oblique subcostal line to increase cephalad and caudad spread to obtain a similar effect. Our study is subject to several important limitations regarding sensory measurement and the termination/regression time of sensory blockade. We measured the effect of TAP blocks using a cold stimulus, rather than postoperative analgesia for pain, because our study subjects were volunteers and were not subjected to abdominal surgery. Cold and pain perceptions are associated with different sensory pathways in terms of receptors, conduction, and central integration. However, a previous study by Børglum et al19 confirmed that pain and cold testing have similar cutaneous areas after TAP block involunteers, and absence of either of these sensations can be used to confirm presence of sensory blockade. Regression of sensory anesthesia may be gradual, and this may make the determination of the actual termination of anesthesia in a particular dermatomal distribution difficult.
A bilateral oblique subcostal TAP block produces a wide spread cutaneous sensory blockade with a consistent dermatomal distribution in the midabdomen for a considerably effective duration in volunteers and may produce an effective alleviation of post operative somatic surgical pain. We encourage our colleagues to pursue further studies using our method under real surgical conditions in order to verify the findings in this study so that we may add another effective intervention/option to our armamentarium of postoperative surgical pain relief.
1. Lee TH, Barrington MJ, Tran TM, Wong D, Hebbard PD. Comparison of
extent of sensory block following posterior and subcostal approaches to
ultrasound-guided transversus abdominis plane block. Anaesth Intensive
Care. 2010;38:452–460.
2. Abdallah FW, Laffey JG, Halpern SH, Brull R. Duration of analgesic
effectiveness after the posterior and lateral transversus abdominis plane
block techniques for transverse lower abdominal incisions: a meta-analysis.
Br JAnaesth. 2013;111:721–735.
3. Walter CJ, Maxwell-Armstrong C, Pinkney TD, et al. A randomised controlled
trial of the efficacy of ultrasound-guided transversus abdominis plane (TAP)
block in laparoscopic colorectal surgery. Surg Endosc. 2013;27:2366–2372.
4. Desmet M, Helsloot D, Vereecke E, Missant C, van de Velde M.
Pneumoperitoneum does not influence spread of local anesthetics in
midaxillary approach transversus abdominis plane block: a descriptive
cadaver study. RegAnesthPainMed. 2015;40:349–354.
5. Rafi AN. Abdominal field block: a new approach via the lumbar triangle.
Anaesthesia. 2001;56:1024–1026.
6. Hebbard P, Fujiwara Y, Shibata Y, Royse C. Ultrasound-guided
transversus abdominis plane (TAP) block. Anaesth Intensive Care.2007;
35:616–617.
7. Arora S, Chhabra A, Subramaniam R, Arora MK, Misra MC, Bansal VK.
Transversus abdominis plane block for laparoscopic inguinal hernia repair:
a randomized trial. JClinAnesth. 2016;33:357–364.
8. Tran TM, Ivanusic JJ, Hebbard P, Barrington MJ. Determination of spread
of injectate after ultrasound-guided transversus abdominis plane block: a
cadaveric study. Br J Anaesth. 2009;102:123–127.
9. Griffiths JD, Middle JV, Barron FA, Grant SJ, Popham PA, Royse CF.
Transversus abdominis plane block does not provide additional benefit to
multimodal analgesia in gynecological cancer surgery. Anesth Analg.2010;
111:797–801.
10. Stoving K, Rothe C, Rosenstock CV, Aasvang EK, Lundstrom LH, Lange
KH. Cutaneous sensory block area, muscle-relaxing effect, and block
duration of the transversus abdominis plane block: a randomized, blinded,
and placebo-controlled study in healthy volunteers. Reg Anesth Pain Med.
2015;40:355–362.
11. Hebbard PD, Barrington MJ, Vasey C. Ultrasound-guided
continuous oblique subcostal transversus abdominis plane blockade:
description of anatomy and clinical technique. RegAnesthPainMed.
2010;35:436–441.
12. ShinHJ, OhAY,BaikJS,KimJH,HanSH,HwangJW.Ultrasound-guided
oblique subcostal transversus abdominis plane block for analgesia after
laparoscopic cholecystectomy: a randomized, controlled, observer-blinded
study. Minerva Anestesiol. 2014;80:185–193.
13. WuY,Liu F, Tang H, et al. The analgesic efficacy of subcostal transversus
abdominis plane block compared with thoracic epidural analgesia and
intravenous opioid analgesia after radical gastrectomy. Anesth Analg.2013;
117:507–513.
14. Li PN, Li H, Wu ML,et al. A cost-effective transparency-based digital imaging
for efficient and accurate wound area measurement. PLoS One. 2012;7:e38069.
15. BasaranB, BasaranA,KozanhanB,KasdoganE,Eryilmaz MA,OzmenS.
Analgesia and respiratory function after laparoscopic cholecystectomy in
patients receiving ultrasound-guided bilateral oblique subcostal transversus
abdominis plane block: a randomized double-blind study. Med Sci Monit.
2015;21:1304–1312.
16. Ghisi D, Fanelli A, Vianello F, et al. Transversus abdominis plane block for
postoperative analgesia in patients undergoing total laparoscopic
hysterectomy: a randomized, controlled, observer-blinded trial. Anesth
Analg. 2016;123:488–492.
17. Oh TK, Yim J, Kim J, et al. Effects of preoperative ultrasound-guided
transversus abdominis plane block on pain after laparoscopic surgery for
colorectal cancer: a double-blind randomized controlled trial. Surg Endosc.
2017;31:127–134.
18. Oksar M, Koyuncu O, Turhanoglu S, Temiz M, Oran MC. Transversus
abdominis plane block as a component of multimodal analgesia for
laparoscopic cholecystectomy. JClinAnesth. 2016;34:72–78.
19. Børglum J, Jensen K, Christensen AF, et al. Distribution patterns,
dermatomal anesthesia, and ropivacaine serum concentrations after
bilateral dual transversus abdominis plane block. Reg Anesth Pain Med.
2012;37:294–301.
