Abstract: Ultrasound-guided interfascial plane blocks are a recent development in modern regional anesthesia research and practice and represent a new route of transmission for local anesthetic to various anatomic locations, but much more research is warranted. Before becoming overtaken with enthusiasm for these new techniques, a deeper understanding of fascial tissue anatomy and structure, aswell asprecise targets for needle placement, is required. Many factors may influence the ultimate spread and quality of resulting interfascial plane blocks, and these must be understood in order to best integrate these techniques into contemporary perioperative pain management protocols.
(Reg Anesth Pain Med 2018;43: 341–346)
Ultrasound has revolutionized the modern practice of regional anesthesia. If we can see it, we can now block it. While the overall number of regional anesthesia techniques described in the ultrasound era has increased, no subset has grown as rapidly as the truncal interfascial plane blocks.1 Although the concept is not new, the reliance on tactile “pops” and “clicks” to identify a needle placement and local anesthetic injection end point has been replaced with direct visualization of fascial planes and other relevant anatomy with ultrasound.1 It seems like a new interfascial plane block is “invented” every month. Arguably, this started with the transversus abdominis plane (TAP) block and has been followed quickly by a series of TAP block derivations (eg, subcostal TAP), Pectoralis nerve (Pecs) I and Pecs II, serratus anterior and quadratus lumborum (QL) blocks, transversalis fascia block, and the erector spinae plane (ESP) block, among others.2–5
Contrary to traditional peripheral regional anesthesia with defined neural end points, the exact targets of the interfascial plane blocks have not been well studied, and the indications are not always well defined. The role of these newer interfascial plane blocks and the goal of introducing them in the context of value-based health care and safe opioid-free pain management are not yet known. In order to interpret the growing literature on interfascial plane blocks and to aid in the design of future studies, a better understanding of the properties of fascial planes is required. The purpose of this Daring Discourse is to bring clarity to the relevant anatomy and function of fascial planes, explain what interfascial plane blocks can and cannot do, and define their role in the contemporary clinical prac tice of regional anesthesia and acute pain medicine.
The fascia is fundamentally composed of soft, collagen containing, loose and dense fibrous connective tissues that perme ate through the whole body.6 Fascial plane structures are not studied well in the anesthesia literature. There are 3 fundamental fascial connective layers in the human body: superficial fascia, deep fascia, and muscle-related fascial layers (epimysium, peri mysium, and endomysium).
The deep fascia is composed of multiple layers and repre sents the target for interfascial plane blocks.7 The deep fascia is a membrane that extends throughout the whole body and is kept under basal tension via numerous muscular attachments. It is de void of fat and forms sheaths for the nerves and vessels and en velops various organs. The deep fascia is independent of the underlying muscle, separated from it by the epimysium and a layer of loose connective tissue (Fig. 1).
Epimysium comprises the densest fascia that encloses each muscle and is continuous with the perimysium and endomysium inside the muscle. It facilitates the muscle sliding movement and is directly involved in the play of tension between the muscles, tendons, and periosteum.8
Continuity of the Fascial System and Migratory Local Anesthetic
Deep fascial planes are potential spaces and act as transmis sion belts around thewhole body across different anatomical locations. Local anesthetic injected within these potential spaces will seek decompressionplanes(ie, “the path of least resistance”). This has been observed in cadaveric studies, even without the contribution of muscle tension. To understand what happens within these tissue planes, we must look for the potential communication routes to appreciate how the anesthetic may spread locally or to more distant locations.9
Unlike peripheral nerve or plexus blocks, interfascial plane blocks may have multiple potential points of injection, and various names have been assigned to blocks in the same tissue plane, al beit between different muscles layers. The best examples of this are the tissue plane of the serratus plane block and Pecs II block. The tissue planes deep to the erector spinae muscle, rhomboid mus cles, serratus anterior muscles, and deep to the latissimus dorsi muscle are the same. Based on the description by Blanco et al,3,10 Forero et al,4 and Elsharkawy et al,11 we speculate that a paraspinal fascial plane block may potentially reach the Pecs II plane (Fig. 2).
It is also possible to target the same continuous fascial plane at different craniocaudal anatomical levels. The ESP block has
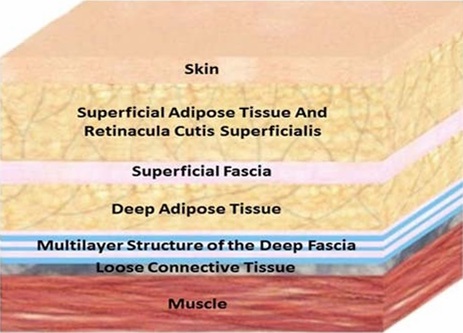
FIGURE 1. Image illustrating the 2 fascial connective layers: superficial fascia and deep fascia. Reproduced with granted permission from Stecco et al.16
been applied to many clinical situations for chest wall analgesia.4 Recently, a low thoracic injection in the ESP has been described for abdominal surgery.12 In the lumbar area, the tissue plane deep to the ESP block is the same tissue plane superficial to the medial posterior aspect of the QL muscle (Fig. 3A).
Another example of this is the anterior QL block, which can be performed at different craniocaudal levels, L4 or L1–2, or subcostal level and various injection sites with individual names (eg, transmuscular QL, transverse oblique paramedian, anterior QL, subcostal QL; Fig. 3B).13–15 The tissue plane between the psoas major muscle and the QL muscle is one continuous tissue plane from L4 to the subcostal levels, and it is continuous cranially to the thoracic paravertebral space deep to the endothoracic fascia.13–15
Biomechanical Properties of Fascia and the Hidden
Role of Fascial Dynamics
The deep fascia has a dynamic property due to multiple factors. First, muscle tendons are often inserted in and attached to these fascial planes causing movement of the planes. Approxi mately 30% ofmuscle forceis transmitted to the connective tissue surrounding muscles. When these muscles contract, they not only move the bones, but they also stretch the deep fascia rendering it mobile.16,17 This stretch or movement of the fascia may result in local anesthetic active transport via a pumping mechanism in addition to passive movement along lower-resistance planes.18,19
Second, fascia may also contain its own contractile elements, which have a role in force generation. This hypothesis is sup ported by in vitro studies demonstrating an autonomous contraction of human lumbar fascia and pharmacological induction of temporary contraction in rat deep fascial tissue.20
Third, fascial layers may also act like anenergy absorber. The thoracolumbar fascia can function as an energy reserve, which is discharged or recharged during every single contraction. Another example is the Achilles tendon and its fascia, which operates like anelastic spring and isabletoabsorb, store,andreleaseenergy.7,21 It is possible that fascial planes, rather than being viewed as rigid, inelastic, and inert structures, may act more like piezoelectric materials of second harmonic generation that convert mechanical forces applied to fascia into energy.22
Tofully understand the clinical effects and role of interfascial plane blocks, we suggest that the biomechanical behavior for each deep fascia be investigated. When viewing interfascial plane blocks through this lens, we find that there are many unanswered
questions. Are the biomechanical properties of fascial tissue and the pumping effect within those fascial planes responsible for the wide but often variable dermatomal effects of a single interfascial injection of local anesthetic? Can differences in biomechanical be havior explain the migration of local anesthetic along fascial planes? Are fascial dynamics, and thus block effects, influenced by anesthetic depth (ie, awake or asleep), the presence or absence of muscle relaxation, or patient positioning (eg, upright vs lateral)?
ROLE OF LOCAL INNERVATION WITHIN THE FASCIAE
With rare exception (eg, ilioinguinal and iliohypogastric nerve blocks), truncal abdominal interfascial plane blocks are taught as not having discrete nerve targets. Recently, however, several studies have highlighted the presence of nerve elements inside fasciae. The results of a human study suggest innervation by both A- and C-fibers. Within fascial tissue, so-called “wide dynamic range” neurons have been found to predominate, which can detect and propagate multiple sensory signals.23 Other groups have observed 2 types of mechanoreceptors—Ruffini corpuscles and Vater-Pacini corpuscles—in the thoracolumbar fascia.24 In addition, some of those nerve elements inside the fascia are adrenergic and potentially control the local blood flow.23 Do these receptors and nerve fibers additionally contribute to the mechanisms of action of interfascial plane blocks? This question, and the potential translation to clinical practice, has yet to be investigated.
NOT ALL FASCIAE ARE THE SAME ( THE CONCEPT OF REGIONAL FASCIAL SPECIALIZATION )
The fascia of each region of the body is specialized and
different in anatomy and function. Specifically, the structure
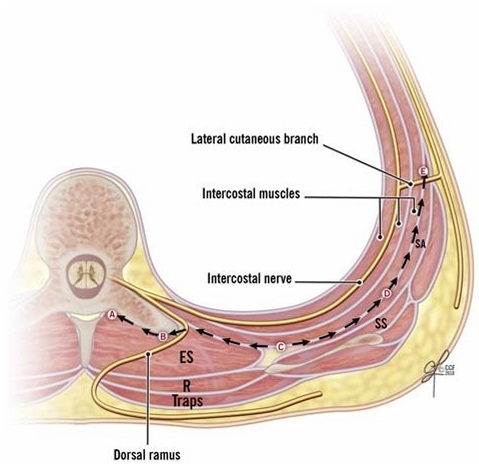
FIGURE 2. Illustration showing a transverse cross section at the T5–T6thoracic level showing thetissue plane deeptotheESmuscle (A, B) as it is continuous laterally with the tissue plane deep to the R muscle (C) and in turn is continuous laterally with the tissue plane deep (D, E) to the SA muscle. A, Location for the retrolaminar block. B, Location for the ES block. C, Location for the rhomboid intercostal block. D and E, Location for the serratus plane block. ES, erector spinae; R, rhomboid; SA, serratus anterior; SS, subscapularis; Traps, trapezius. Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography © 2018. All Rights Reserved.
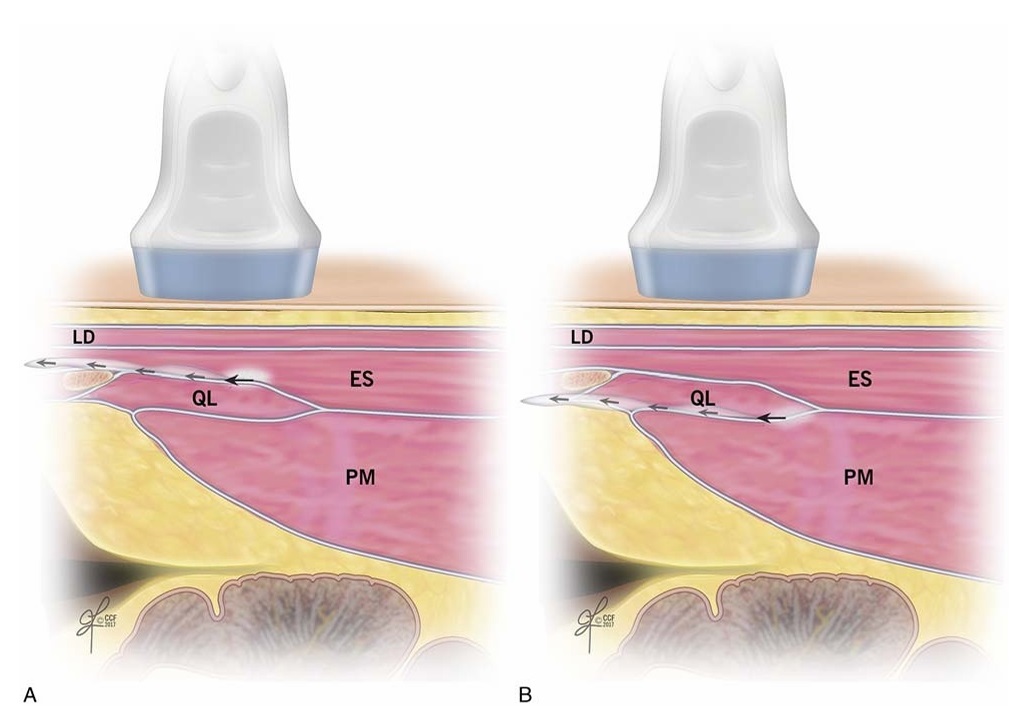
FIGURE 3. A,Illustration showing a sagittal section of the tissue plane deep to the ES muscle, as it is continuous caudally with the tissue plane superficial to the medial posterior aspect of the QL muscle. B, Illustration showing a sagittal section of the tissue plane between the PM muscle and the QL muscle as one continuous tissue plane from L4 to the subcostal level, and it is continuous cranially to the thoracic paravertebral space deep to the endothoracic fascia. ES, erector spinae; LD, latissimus dorsi; PM, psoas major; QL, quadratus lumborum. Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography © 2018. All Rights Reserved.
of the deep fascial plane appears to vary by location. Differ ences between the deep fasciae of the limbs and of the trunk have been described. These differences are due to the number of the layers, function, and relationships with surrounding or gans,25 a concept that can be considered regional fascial specialization, and need to be considered when evaluating a new interfascial block technique.
Differences in Number of Layers
The deep fasciae of the chest wall (pectoral region) are usu ally formed by a single layer of undulated collagen and elastic fibers adhering to the underlying muscles,16 whereas the deep fasciae of the limbs are formed of 2 or 3 sublayers of parallel collagen fiber bundles. For example, in the thigh, the deep fascia is independent of the underlying muscle, separated by the epimysium and a layer of loose connective tissue.26 The existence of sublayers, and varying in number, inside the thoracolumbar fascia has been described. The middle thoracolumbar fascia contains 3 sublayers (Fig. 4).27 The number and distinction of the fascial layers usually cannot be clearly defined using current ultrasound technology. In addition, it is not yet known if there is an optimal choice of layer for local anesthetic injection or whether this choice will affect the spread of medication or clinical outcome.
Differences in Fascial Function
Some fascial layers are more mobile than others, and this maytranslate into more diffusion ofthe LA.Whenlookingclosely at the deep fascia of the pectoral region, the pectoralis fascia acts as an additional insertion for the pectoralis major muscle, which makes it more mobile than others.28 The thoracolumbar fascia is more mobile than other fasciae. In the middle thoracolumbar region, the fascia connects laterally to the muscles of the lateral ab dominal wall and attaches medially to the tips of the transverse processes, so it acts more like a tendon.27
Differences in Fascial Relationships With Surrounding Organs
Thesurrounding organs of the deep fascia differ by anatomical location and may have clinical relevance, although this issue has yet to be explored. Do the presence and location of organs around specific fascial layers affect the spread of local anesthetic? For example, when performing blocks involving the thoracolumbar fascia, do the relevant organs (eg, liver on the right and spleen on the left) influence the cranial local anesthetic spread and the extent of der matomal coverage? It is conceivable that the cranial anesthetic spread may be impeded on the right side of the body by the presence of the liver. Is this clinically relevant? Can interfascial block ade and local anesthetic spread in the thorax be influenced by the presence of negative or positive intrathoracic pressure (ie, spontane ous ventilation vs positive pressure ventilation)?

FIGURE 4. Illustration showing the middle thoracolumbar fascia (MTLF) at L4 level and its sublayers; the MTLF contains 3 layers. The circle shows a magnified detailed image of the 3 layers of the MTLF: (1) the red dashed line encircling the QL muscle represents the epimysium-investing fascia of QL; (2)the white layer between the 2 colored dashed linesrepresents the aponeurosisofthe IO andTAmuscles; (3) the blue dashed line represents the deep lamina of the posterior layer of the thoracolumbar fascia encircling the erector spinae (ES) muscle. EO, external oblique muscle; IO, internal oblique; LIFT, lumbar interfascial triangle; PM, psoas major; QL, quadratus lumborum, latissimus dorsi; TA, transversus abdominis. Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography © 2018. All Rights Reserved.
Ultimately, the role of new regional anesthesia techniques should be to increase patient access to safe opioid-free pain relief. Although paravertebral blocks have been a well-established tech nique for perioperative pain management after breast and thoracic surgery, their rate of use remains low for various reasons.29 The emergence of interfascial plane blocks for the same surgical in dications, facilitated by ultrasound and with arguably less severe complications associated with them, has the potential to achieve greater patient access to regional analgesia. For major abdominal surgery, epidural analgesia continues to be the criterion standard; unlike an epidural infusion, current common approaches for interfascial plane blocks do not match the visceral coverage or duration of analgesia.1 However, surgical practices are also changing, and with these changes, the demand for epidural analgesia is being questioned. Surgeons’ preferences have started to shift away because of enhanced recovery protocols emphasizing minimally invasive surgical techniques, earlier mobility, and lower levels of intravenous fluid administration. Rather than re moving patient access to local anesthesia as part of a multimodal regimen for perioperative pain management, with practices moving away from epidurals, use of interfascial plane blocks may represent one alternative to provide continued regional analgesia. Advances in extended-release local anesthetic compounds or using catheters with the developments in infusion and intermittent bolus technology may overcome current limitations on duration. When interfascial plane blocks are used in the context of multimodal analgesia with other nonopioid pain medications (including systemic local anesthetics and nonsteroidal anti inflammatory drugs) and opioids, they may better address the multifaceted pain experience. In this context, even if the analge sia provided by interfascial plane blocks in this region is not equivalent to an epidural, perhaps being noninferior is sufficient. Experts currently suggest that aggressive treatment of acute pain mayhavepotential benefits in preventing the transition to persistent postsurgical pain.30–32
Through this Daring Discourse, we hope to not only raise awareness to the limitations of our current knowledge but also suggest future research directions and other opportunities to fill these gaps. The highest priority areas in the study of interfascial plane blocks include anatomy, function, access, and outcomes. In terms of anatomic knowledge, a combination of histologic and gross anatomic studies is applicable. Given the differences in numberoflayers within the fasciae according to anatomic site27 and location of neural elements within the fasciae,23,24 we believe there is a need for detailed microanatomy research to better under stand the ideal location for local anesthetic injection, and as well as where and why local anesthetic spreads the way it does. Methods used to study the microanatomy of nerves (eg, electron microscopy, optical projection tomography) may beuseful.33,34 Is sues related to the spread of local anesthetic and the potential in fluence of neighboring organs and sidedness may be explored to some degree through human cadaver studies. Using methodology described previously,15–35 patterns of dye spread with compari sons of left- and right sided injections within a sample of human cadavers require further investigation. Further, the potential effects of port placement during laparoscopy and air infiltration within the abdominal wall layers on the pattern of dye spread following interfascial plane block remain to be studied in a cadaver model. Arguably these regional effects (eg, sidedness, proximity to neigh boring organs) need to be studied for each of the new truncal interfascial plane blocks. In terms of function, the biomechanical properties of fascial layers and potential effects on local anesthetic spread likely require studies using a living animal model and/or human participants. This is where cadaver research is not always di rectly applicable. Local anesthetic spread during spontaneous versus mechanical ventilation with or without pharmacologic muscle relaxation may be studied using either of these study designs. In hu man volunteers, perhaps the effects of voluntary activity (eg, Valsalva maneuver, positioning, physical activity, or simulated physical therapy) on the pattern of local anesthetic spread may be mapped using clinical bedside imaging similar to a previously published study.36 In terms of assessing access and outcomes of interfascial plane blocks, there may be rolefor “big data” research. Despite plenty of supporting evidence, we know that the overall utilization of regional anesthesia techniques in the perioperative management of pain continues to remain low even for common surgeries. For patients who undergo truncal abdominal, thoracic, or breast surgery, the rise in interfascial plane blocks should repre sent an effective means to increase access to regional analgesic techniques. Over time, retrospective cohort studies using registries or administrative databases37–39 may be able to measure changes in the rate of utilization of regional analgesia for these patients, if any. We expect that there will continue to be challenges in proving long-term outcomes benefits of regional anesthesia and analgesia techniques, and this issue is not limited to interfascial plane blocks. Regional anesthesia and analgesia typically do not take place in a vacuum, and other factors (eg, patient, procedure, provider) routinely modify outcomes. Interfascial plane blocks represent one element of multimodal analgesia for patients having truncal surgery, which, as a bundle, may have benefits to patients in the short and long term; investigators designing prospective studies may wish to focus on outcomes related to the clinical pathway and not one individual element. Clinically meaningful outcomes, those that add value according to the Triple Aim, will improve health, enhance the patient experience, and decrease costs.40 Regional anesthesiolo gists and researchers should recognize the opportunity to apply their skills in the personalization of pain medicine and measure out comes that are important to patients.41,42
CONCLUSIONS
Ultrasound-guided interfascial plane blocks are a recent de velopment in modern regional anesthesia research and practice and represent a new route of transmission for local anesthetic to various anatomic locations, but much more research is warranted. Before we become overtaken with enthusiasm for these new techniques, we need to go back to basics by deepening our understanding of fascial tissue anatomy and structure and determine the precise targets for needle placement. This an important area for future research because, rather than identifying a precise nerve lo cation with predictable effects of local anesthetic on a target nerve or plexus, interfascial plane blocks require assessing the location of fascial planes in different regions of the body, unpredictable spread of LA across tissue planes (not confined to small area), and unknown potential implications on patient outcomes. We also need an elevated understanding of the many factors that influence the ultimate spread and quality of the resulting block in order to best integrate them into contemporary perioperative pain management protocols.
ACKNOWLEDGMENTS
The authors thank Dr Richard Rosenquist for supporting the work presented in this article.
1. Chin KJ, McDonnell JG, Carvalho B, Sharkey A, Pawa A, Gadsden J.
Essentials of our current understanding: abdominalwall blocks.Reg Anesth
Pain Med. 2017;42:133–183.
2. Blanco R. Tap block under ultrasound guidance: the description of a “no
pops” technique. Reg Anesth Pain Med. 2007;32:130.
3. BlancoR,Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: a
novel ultrasound-guided thoracic wall nerve block. Anaesthesia.2013;68:
1107–1113.
4. Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae
plane block: a novel analgesic technique in thoracic neuropathic pain.
RegAnesthPainMed. 2016;41:621–627.
5. Hebbard PD. Transversalis fascia plane block, a novel ultrasound-guided
abdominal wall nerve block. Can J Anaesth.2009;56:618–620.
6. Adstrum S, Hedley G, Schleip R, Stecco C, Yucesoy CA. Defining the
fascial system. JBodywMovTher.2017;21:173–177.
7. KlinglerW,Velders M,HoppeK,PedroM,SchleipR.Clinicalrelevanceof
fascial tissue and dysfunctions. Curr Pain Headache Rep. 2014;18:439.
8. Findley T, Chaudhry H, Stecco A, Roman M. Fascia research—a narrative
review. JBodywMovTher.2012;16:67–75.
9. Wilke J, Krause F, Vogt L, Banzer W. What is evidence-based about
myofascial chains: a systematic review. Arch Phys Med Rehabil.2016;97:
454–461.
10. Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of Pecs
II (modified Pecs I): a novel approach to breast surgery. Rev Esp Anestesiol
Reanim. 2012;59:470–475.
11. Elsharkawy H, Saifullah T, Kolli S, Drake R. Rhomboid intercostal block.
Anaesthesia. 2016;71:856–857.
12. Chin KJ, Adhikary S, Sarwani N, Forero M. The analgesic efficacy of
pre-operative bilateral erector spinae plane (ESP) blocks in patients having
ventral hernia repair. Anaesthesia. 2017;72:452–460.
13. Dam M,Hansen CK, Børglum J, Chan V, Bendtsen TF. A transverse
oblique approach to the transmuscular quadratus lumborum block.
Anaesthesia. 2016;71:603–604.
14. El-Boghdadly K, Elsharkawy H, Short A, Chin KJ. Quadratus lumborum
block nomenclature and anatomical considerations. RegAnesthPainMed.
2016;41:548–549.
15. Elsharkawy H, El-Boghdadly K, Kolli S, et al. Injectate spread following
anterior sub-costal and posterior approaches to the quadratus lumborum
block: a comparative cadaveric study. Eur J Anaesthesiol.2017;34:
587–595.
16. Stecco C, Macchi V, Porzionato A, Duparc F, de Caro R. The fascia: the
forgotten structure. Ital J Anat Embryol. 2011;116:127–138.
17. Yucesoy CA, Maas H, Koopman BH, Grootenboer HJ, Huijing PA.
Mechanisms causing effects of muscle position on proximo-distal muscle
force differences in extra-muscular myofascialforce transmission. Med Eng
Phys. 2006;28:214–226.
18. Lelean P. The migratory fascia hypothesis. JBodywMovTher.2009;13:
304–310.
19. Stecco C, Gagey O, Belloni A, et al. Anatomy of the deep fascia of the upper
limb. Second part: study of innervation. Morphologie. 2007;91:38–43.
20. Condino S, Turini G, Parrini S, et al. A semiautomatic method for in vivo
three-dimensional quantitative analysis of fascial layers mobility based on
3Dultrasound scans. Int J Comput Assist Radiol Surg.2015;10:
1721–1735.
21. Sawicki GS, Lewis CL, Ferris DP. It pays to have a spring in your step.
Exerc Sport Sci Rev. 2009;37:130–138.
22. Rivard M, Laliberte M, Bertrand-Grenier A, et al. The structural origin of
second harmonic generation in fascia. Biomed Opt Express. 2010;2:26–36.
23. Bednar DA, Orr FW, Simon GT. Observations on the pathomorphology of
the thoracolumbar fascia in chronic mechanical back pain. A microscopic
study. Spine (Phila Pa 1976). 1995;20:1161–1164.
24. Benetazzo L, Bizzego A, de Caro R, Frigo G, Guidolin D, Stecco C. 3D
reconstruction of the crural and thoracolumbar fasciae. Surg Radiol Anat.
2011;33:855–862.
25. Benjamin M. The fascia of the limbs and back—areview.JAnat. 2009;
214:1–18.
26. Stecco A, Macchi V, Masiero S, et al. Pectoral and femoral fasciae: common
aspects and regional specializations. Surg Radiol Anat. 2009;31:35–42.
27. Willard FH, Vleeming A, Schuenke MD, Danneels L, Schleip R. The
thoracolumbar fascia: anatomy, functionand clinicalconsiderations. JAnat.
2012;221:507–536.
28. Loukas M, Shoja MM, Thurston T, Jones VL, Linganna S, Tubbs RS.
Anatomy and biomechanics of the vertebral aponeurosis part of the posterior
layer of the thoracolumbar fascia. Surg Radiol Anat. 2008;30:125–129.
29. Duale C, Gayraud G, Taheri H, Bastien O, Schoeffler P. A French
nationwide survey on anesthesiologist-perceived barriers to the use of
epidural and paravertebral block in thoracic surgery. J Cardiothorac Vasc
Anesth. 2015;29:942–949.
30. Richebe P, Julien M, Brulotte V. Potential strategies for preventing chronic
postoperative pain: a practical approach: continuing professional
development. Can J Anaesth. 2015;62:1329–1341.
31. Clarke H, Katz J, Flor H, Rietschel M, Diehl SR, Seltzer Z. Genetics of
chronic post-surgical pain: a crucial step toward personal pain medicine.
Can JAnaesth. 2015;62:294–303.
32. Bayman EO, Parekh KR, Keech J, Selte A, Brennan TJ. A prospective study
of chronic pain after thoracic surgery. Anesthesiology. 2017;126:938–951.
33. Brull R, Hadzic A, Reina MA, Barrington MJ. Pathophysiology and
etiology of nerve injury following peripheral nerve blockade. Reg Anesth
Pain Med. 2015;40:479–490.
34. Cvetko E, Capek M, Damjanovska M, Reina MA, Erzen I, Stopar-Pintaric
T. The utility of three-dimensional optical projection tomography in nerve
injection injury imaging. Anaesthesia. 2015;70:939–947.
35. Barrington MJ, Ivanusic JJ, Rozen WM, Hebbard P. Spread of injectate
after ultrasound-guided subcostal transversus abdominis plane block: a
cadaveric study. Anaesthesia. 2009;64:745–750.
36. Stoving K, Rothe C, Rosenstock CV, Aasvang EK, Lundstrom LH, Lange
KH. Cutaneous sensory block area, muscle-relaxing effect, and block
duration of the transversus abdominis plane block: a randomized, blinded,
and placebo-controlled study in healthy volunteers. RegAnesthPainMed.
2015;40:355–362.
37. Cozowicz C, Poeran J, Memtsoudis SG. Epidemiology, trends, and
disparities in regional anaesthesia for orthopaedic surgery. Br J Anaesth.
2015;115(suppl 2):ii57–ii67.
38. Masaracchia MM, Herrick MD, Barrington MJ, Hartmann PR, Sites
BD. Adductor canal blocks: changing practice patterns and
associated quality profile. Acta Anaesthesiol Scand. 2017;61:
224–231.
39. Gabriel RA, Kaye AD, Nagrebetsky A, Jones MR, Dutton RP, Urman RD.
Utilization of femoral nerve blocks for total knee arthroplasty.
J Arthroplasty. 2016;31:1680–1685.
40. Berwick DM, Nolan TW, Whittington J. The Triple Aim: care, health, and
cost. Health Aff (Millwood). 2008;27:759–769.
41. Morgan SJ, Friedly JL, Amtmann D, Salem R, Hafner BJ.
Cross-sectional assessment of factors related to pain intensity and pain
interference in lower limb prosthesis users. Arch Phys Med Rehabil.
2017;98:105–113.
42. De Oliveira GS Jr, Fitzgerald PC, Marcus RJ, Ahmad S, McCarthy RJ. A
dose-ranging study of the effect of transversus abdominis block on
postoperative quality of recovery and analgesia after outpatient
laparoscopy. Anesth Analg. 2011;113:1218–1225.
