Abstract: We performed a systematic search of the medical literature and reviewed the evidence examining success rates and incidence of complications of ultrasound (US) guidance relative to traditional tech niques for the following blocks: paravertebral, intercostal, transversus abdominis plane, rectus sheath, and ilioinguinal/iliohypogastric. We in cluded studies of sufficient methodologic quality for review and ex cluded poor-quality studies. We then rated the strength of evidence for US guidance for each block using a system developed by the United States Agency for Health Care Policy and Research. Although relatively few studies have compared US guidancewith established techniques, the available evidence suggests that the use of US guidance is a safe and effective means to facilitate correct needle placement and adequate spread of local anesthetic for truncal blocks. Further studies are needed to directly compare US guidance to traditional techniques and to clarify potential benefits and limitations of US guidance for truncal blocks.
(Reg Anesth Pain Med 2010;35: S36YS42)
Anesthesia and/or analgesia of the trunk can be achieved with perineural injections, which have several advantages com pared with neuraxial blockade. These include reduced sympa the ctomy,1 less severe consequences of infection or bleeding at the injection site,2Y4 minimal interference with bladder and bowel function,1,5 and decreased incidence of lower extremity motor weakness,6Y8 allowing early ambulation and home discharge.
Thoracic paravertebral or intercostal nerve blocks (ICNBs) of T1 to T6 can provide anesthesia and/or analgesia of the chest wall. Thoracic paravertebral blocks from T6 to L1, transversus abdominis plane (TAP) blocks, rectus sheath blocks, or ilioin guinal (II)/iliohypogastric (IH) nerve blocks can provide anesthe
sia and/or analgesia of the abdominal wall. Recent developments including refinements in continuous catheter techniques and use of ultrasound (US) guidance have increased the clinical applications for truncal blocks. We sought to review the evidence for US guidance for truncal blocks and make recommendations for use of US based on the strength of available data.
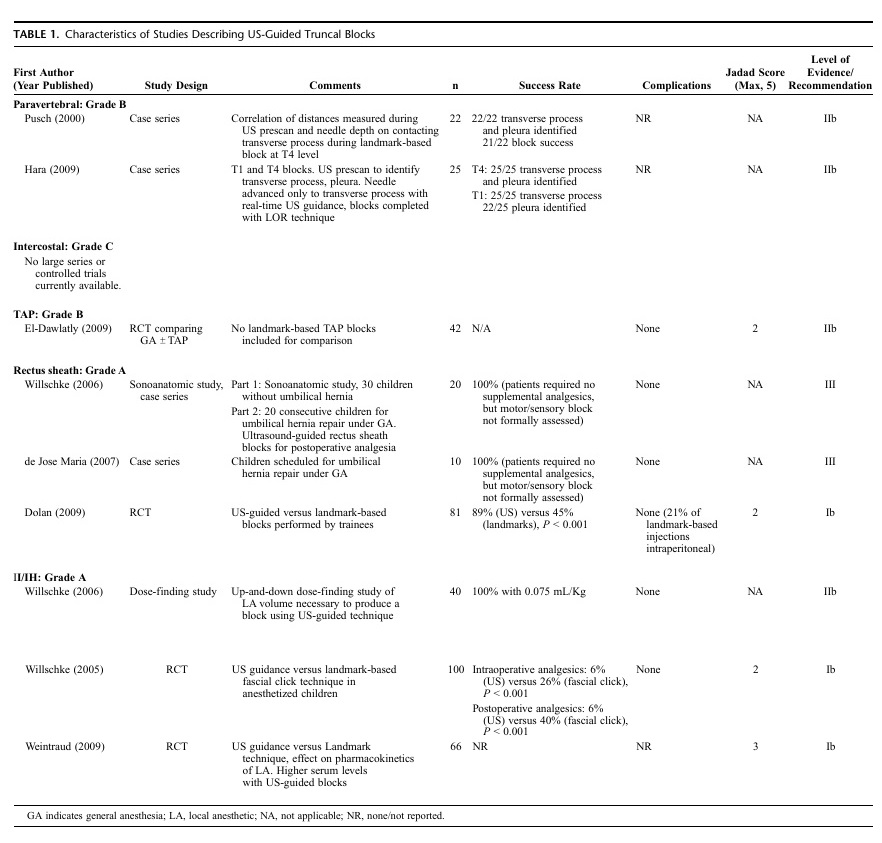
We systematically searched MEDLINE, the Cochrane Central Register of Controlled Trials, Ovid, and Google Scholar databases for articles published between January 1, 1990, and August 1, 2009, using the following keywords: ultrasound with paravertebral, intercostal, transversus abdominis plane, TAP, rectus sheath, ilioinguinal, and iliohypogastric. We then searched the references of eligible articles for additional studies. Ran domized controlled trials, nonrandomized experimental studies, and large case series were included for review. Case reports, small case series (G10 patients), and letters to the editor were excluded. Because of the limited amount of published data, cadaver ana tomic studies and letters reporting significant findings were in cluded for discussion. However, these were not used for making evidence-based recommendations. Methodologic quality of the studies included was rated using a validated scoring system de scribed by Jadad et al.9 For all of the blocks we evaluated, the evidence examining use of US guidance was rated using an evidence-based system developed by the United States Agency for Health Care Policy and Research. A summary of studies pertaining to US guidance for these truncal blocks is shown below in Table 1.
Thoracic Paravertebral Blocks
Background
Thoracic paravertebral blocks have been used to provide surgical anesthesia for many types of surgical procedures involving the chest and/or abdomen,10 Y 18 as well as to provide analgesia for painful conditions such as rib fractures.19Y22 In addition, paravertebral blocks may be associated with a decreased rate of recurrence after surgical excision of malignant breast lesions.23 Specific risks of paravertebral blocks include epidural 24 or intra the cal 25 spread of anesthetic, systemic local anesthetic toxicity, 26 and hemo/pneumothorax.27Y29 Standard techniques use surface landmarks and can be combined with either nerve stimulation or loss-of-resistance (LOR).30Y32 Although US visualization of the paravertebral space may be challenging owing to the overlying bony structure such as the ribs and transverse processes, use of
USto measure the distance from skin to the transverse processes or for real-time image guidance during needle placement could potentially decrease the risk of puncturing the pleura with the needle during block placement.
Ultrasound Data
There is a paucity of data on US guidance for the thoracic paravertebral block. Recently, Pusch et al33 demonstrated that the depth of the transverse process and the pleura could be reliably measured at T4 before block placement in a series of 22 patients. More recently, Hara et al34 reported a cohort study of 25 patients who underwent an US-guided paravertebral injection at T4 and T1 with 25 of 25 and 22 of 25 successful blocks, respectively. However, they only imaged the needle until the transverse process was contacted, then continued needle advancement using an LOR technique. Luyet et al35 studied the placement of catheters in the paravertebral space of cadavers. Twenty catheters were placed in 10 cadavers, and placement was confirmed by evaluating the spread of contrast dye using computed tomography. Although the paravertebral space was easy to visualize and placement of the needle tip within this space was accomplished easily, contrast injected through the catheters was frequently (9/20 catheters) visualized in the pleural, epidural, or prevertebral spaces. The catheters used in this study were styleted and advanced 5 cm past the needle tip. To date, no randomized controlled trial (RCT) has compared US guidance to conventional techniques such as anatomic land marks, LOR, or nerve stimulation for placement of either single shot or continuous paravertebral blocks.
Recommendations
We give a Grade B recommendation for the use of US to place paravertebral blocks, based on Level IIb (2 small case series) evidence. The available literature suggests that thoracic para vertebral blocks may be performed with a high probability of block success using US guidance as an adjunct to traditional techniques. The use of styleted catheters or blind advancement of the catheter more than 2 cm past the needle tip may contribute to catheter misplacement during US-guided placement of tho racic paravertebral catheters (based on results of 1 cadaver ana tomic study). At this time, there is insufficient evidence to show that US guidance improves block success rates or reduces the risk of complications compared with traditional techniques for performing single-shot or continuous paravertebral blocks.
Intercostal Nerve Blocks
Background
Intercostal nerve blocks are most commonly used as an al ternative to epidural or paravertebral block to provide analgesia for painful conditions of the chest wall or after thoracic or upper abdominal surgery.36Y39 Risks of ICNBs are similar to those for thoracic paravertebral blocks.40Y48 Traditional techniques for performing ICNBs generally involve use of surface anatomic landmarks to guide needle placement.49 Although the intercostal neurovascular bundle may not be visualized with US owing to
acoustic shadowing from the overlying rib, use of US guidance could be useful for performing ICNBs because imaging the pleura and needle tip in real-time potentially could reduce the risk of puncturing the pleura during block placement.
Ultrasound Data
There are minimal data available for US-guided ICNBs. One small descriptive case series (4 patients)50 has reported success ful use of US-guided cryoablation of intercostal nerves to treat chronic postthoracotomy pain. To date, no RCTs or large case series have been published to report success rates or the rate of complications for US-guided ICNBs or to compare US guidance with traditional techniques.
Recommendations
Onthebasis of the minimal available Level III (1 very small case series) evidence, we give US guidance for ICNB a Grade C recommendation. At this time, there is insufficient evidence to comment on the rates of block success or complications for US-guided ICNBs relative to those performed using traditional techniques. Thus far, the literature only establishes proof of the concept that US guidance can be used to perform ICNBs.
Transversus Abdominis Plane Blocks
Background
The ventral rami of spinal nerve roots T6-L1 course through the lateral abdominal wall within a potential space defined superiorly by the costal margin, inferiorly by the iliac crest, medially by the lateral border of the rectus abdominis muscle, superficially by the internal oblique muscle, and deep by the transversus abdominis muscle. Rafi51 first described in 2001 a landmark-based technique of accessing this TAP percutaneously via the lumbar triangle of Petit to deposit local anesthetic solution and produce analgesia of the anterolateral abdominal wall. The landmark-based technique relies on a B2-pop[ end point to determine correct positioning of the needle tip beneath the fascia
overlying the transversus abdominis muscle.52 The primary indication for the TAP block is to provide analgesia after major surgical procedures of the anterolateral abdominal wall.53Y56 To date, use of the TAP block for surgical anesthesia has not been reported.
Intraperitoneal catheter placement without both visceral organ injury 57 and liver injury from the block needle 58 has been reported for TAP blocks performed using traditional techniques. Because US-guided techniques allow real-time visualization of the needle and the spread of local anesthetic, the use of US may decrease the risk of complications for the TAP block. In addition, an in-plane US-guided approach may confirm additional safety because it involves an oblique needle trajectory, possibly decreasing the risk of advancing the needle into the peritoneal cavity.
Ultrasound Data
In a cadaver study, Tran et al59 demonstrated that the spread of injectate was limited to the T9-L1 nerve roots for US-guided TAP blocks performed at a level similar to that for traditional techniques. Shibata et al60 and Hebbard61 performed separate retrospective audits of patients with US-guided TAP blocks and suggested that traditional TAP blocks may not reliably provide analgesia for procedures above the level of the umbilicus. However, traditional techniques may eventually result in blocks extending as high as the T7 dermatomal level owing to Bextensive communication between adjacent segmental thora columbar nerves.[62 Hebbard61 described a modified subcostal US-guided approach and reported a mean block height of 85% the distance from the symphysis pubis to the xiphoid process in a series of 26 patients.
El-Dawlatly et al56 recently described a technique for US guided TAP block that is essentially identical to those previously reported.60,63,64 In addition, they performed an RCT comparing intraoperative narcotic requirements and postoperative analgesia in patients undergoing laparoscopic cholecysectomy with and without bilateral TAP blocks. They found that patients with TAP blocks had substantially lower perioperative opioid consumption than patients in the control group. However, this study did not include any patients with TAP blocks performed using traditional techniques for comparison. To date, no study has directly compared landmark-based approaches with US-guided techniques. At this time, no complications have been reported for US-guided TAP blocks.
Recommendations
We give US guidance for TAP blocks a Grade B recommendation based on available Level IIb (1 RCT, no traditional technique TAP block group included for comparison) evidence.
At this time, no definitive statements can be made with regard to the rate of block failure or complications from US-guided TAP blocks relative to those performed using traditional tech niques. However, the existing case series do indicate high success rates for TAP blocks performed with US guidance. Although no prospective clinical studies have directly compared traditional (landmark-based or US-guided) to subcostal approaches to the TAP, case series (2 small series), and anatomic studies (1 cadaver study) suggest differences in the distribution of sensory blockade for the various approaches.
Rectus Sheath Blocks
Background
The central portion of the anterior abdominal wall is innervated by the ventral branches of spinal nerve roots T6-L1, which lie between the belly of the rectus abdominis muscle and the posterior rectus sheath and enter the rectus muscle near the midline. The superior and inferior epigastric vessels run longi tudinally through the medial portion of the muscle. The tendinous intersections of the rectus muscle are not fused to the posterior rectus sheath, which allows local anesthetic to spread cephalocaudad within the ipsilateral compartment from a single injection site.
The rectus sheath block has been used to provide surgical anesthesia as well as postoperative analgesia for surgical pro cedures involving a vertical midline laparotomy incision as well as for laparoscopic procedures.65Y67 Traditionally, this block is performed using Bpops[ or Bscratching sensations[ to determine proper positioning of the needle’s tip. Potential advantages of US guidance for rectus sheath blocks are similar to those for TAP blocks.
Ultrasound Data
Few data exist regarding the use of US guidance for rectus sheath blocks. Willschke et al68 and de Jose Maria et al69 reported case series of 20 and 10 pediatric patients, respectively. Patients in both series had rectus sheath blocks placed for postoperative
analgesia after abdominal surgery performed under general an esthesia. Both groups reported 100% success in the ability to visualize the spread of anesthetic between the belly of the rectus abdominis muscle and the posterior rectus sheath. Although neither study formally assessed the patients for motor or sensory block, no patient in either series required additional analgesic medication during surgery or before discharge home. No com plications were reported for either series.
Recently, Dolan et al70 performed an RCT comparing the accuracy of local anesthetic deposition during rectus sheath blocks performed by trainees using either LOR or US guidance. They found that anesthetic was placed in the correct plane in only 45% of cases using LOR and in 89% of cases using US guid ance (P G 0.001). In addition, this difference between groups became more pronounced as patient body mass index increased. Of additional concern was their finding that 21% of blocks performed using LOR had an initial anesthetic injection deep to the rectus sheath (intraperitoneal). Although no complication resulted, they stopped the trial after enrollment of 81 patients because of their concern for potential intra-abdominal injury with blocks performed using LOR. However, this frequency of intraperitoneal injection may not be representative of that for practitioners with extensive experience performing rectus sheath blocks using traditional techniques as all blocks in this study were performed by trainees with no previous experience performing rectus sheath blocks using either US or LOR.
Recommendations
Wegive use of US guidance for rectus sheath block a Grade Arecommendation based on available Levels Ib (1 RCT) and III (2 small case series) evidence. The current evidence indicates that US guidance is more likely than traditional techniques to produce a successful block. Although the studies conducted to date lack statistical power to demonstrate any safety advantage conferred by use of US, the high rate of intraperitoneal injection observed during blocks performed using traditional techniques is con cerning. More RCTs involving more patients will help to clarify the potential benefits and limitations of US guidance for rectus sheath blocks.
Ilioinguinal/Iliohypogastric Nerve Blocks
Background
The II nerve provides sensation to the upper medial part of the thigh and the upper part of thegenitalia. The IH nerve provides sensation to the buttock and abdominal wall above the pubis. Traditional landmark-based techniques vary but share a theme of relying on facial Bclicks.[71 Traditional techniques may be unreliable, however, because US imaging has demonstrated infrequent placement of local anesthetic around the intended muscle planes and nerves after landmark-based II/IH blocks in children.72
Most II and IH blocks are placed for analgesia after inguinal hernia repair, often in children. The II/IH blocks have also been shown to provide similar analgesia to caudal blocks during orchidopexy73,74 while eliminating adverse effects of motor block and urinary retention. The II and IH blocks have been also successfully used to provide surgical anesthesia for herniorrhaphy and to improve analgesia following a variety of lower abdominal procedures in adults.75Y79 Risks specific to the II/IH block include bowel hematoma,80 bowel puncture,81,82 pelvic he matoma,83 femoral nerve block,84,85 and high serum local anes thetic concentration.86,87 Potential advantages of US guidance for II/IH blocks are similar to those for rectus sheath and TAP
blocks.
Ultrasound Data
One RCT has been conducted comparing US guidance to a landmark-based technique.88 One hundred children scheduled for inguinal hernia, orchidopexy, or hydrocele repair under general anesthesia were prospectively randomized to receive either US guided or landmark-based II/IH blocks for postoperative analge sia. Because formally assessing motor and sensory block can be difficult in young children, the authors used validated, predefined, objective parameters to guide administration of supplemental analgesics during surgery (increase in heart rate or mean arterial pressure 910%) and postoperatively (the objective pain scale, a validated measure of objective behavioral variables). They reported statistically significant differences in the number of patients responding to surgical incision (6% US group versus 22% fascial click group, P G 0.0001) and requiring supplemental analgesic medication during recovery (6% US group versus 40% fascial click group, P G 0.0001). Upon US scanning of patients whohad received blocks by the fascial click method, only 50% of those patients demonstrated LA deposited around the II/IH nerves compared with 100% in the US group. It is important to note that for this study, the anesthesiologists were not blinded to patient group allocation, creating a potentially significant source of bias. The same group of investigators also conducted a dose comparison analysis using an up-and-down dosing method to determine the amount of local anesthetic necessary to achieve complete success in an interventional group.89 They demonstrated an effective local anesthetic dose of 0.075 mL/kg for US-guided blocks compared with standard doses of 0.3 to 0.5 mL/kg for landmark-based II/IH blocks.
Although reduced amounts of local anesthetic may be necessary to perform II/IH blocks, serum levels of local anes thetic may be higher for US-guided blocks. In a controlled study, Weintraud et al90 describe higher serum ropivicaine levels in US-guided patients receiving equal amounts of local anesthetic to those receiving landmark-based blocks. Therefore, it is prob ably warranted to reduce the volume of local anesthetic when performing US-guided II/IH blocks because less local anes
thetic is necessary to achieve successful blocks, and there may be a higher serum absorption of local anesthetic, possibly be cause local anesthetic is often deposited near a perforating branch of the deep circumflex iliac artery using an US-guided technique.
Recommendations
We give the use of US for II/IH blocks a Grade A rec ommendation based on available Levels Ib (2 RCTs) and IIb (1 dose-finding study) evidence. The available data indicate that compared with traditional techniques, US-guided II/IH blocks have a higher probability of block success and require a lower volume of local anesthetic. However, there are currently not enough data to demonstrate any safety advantage for US guidance over traditional techniques. Ultrasound-guided II/IH blocks may also result in higher plasma concentrations than those performed with traditional techniques using similar volumes of local anesthetic.
Relatively few large studies have been conducted to evaluate the role of US guidance for truncal blocks. Only 2 prospective RCTs have been performed to compare US guidance to standard landmark-based approaches, so at this time, no definitive state ments can be made regarding improvements in success rates or reductions in the frequency of complications. The strongest evi dence in favor of US guidance for truncal blocks is for II/IH and rectus sheath blocks. There is sparse evidence in favor of US guidance for TAP blocks and minimal evidence to support US guidance for thoracic paravertebral and ICNBs. Further studies are required to clarify the potential benefits of US guidance for truncal blocks.
