Background and Objectives: The erector spinae plane (ESP) and retrolaminar blocks are ultrasound-guided techniques for thoracoabdominal wall analgesia involving injection into the musculofascial plane between the paraspinal back muscles and underlying thoracic vertebrae. The ESP block targets the tips of the transverse processes, whereas the retrolaminar block targets the laminae. We investigated if there were differences in injectate spread between the 2 techniques that would have implications for their clinical effect.
Methods: The blocks were performed in 3 fresh cadavers. The ESP and retrolaminar blocks were performed on opposite sides of each cadaver at the T5 vertebral level. Twenty milliliters of a radiocontrast dye mixture was injected in each block, and injectate spread was assessed by magnetic resonance imaging and anatomical dissection.
Results: Both blocks exhibited spread to the epidural and neural foraminal spaces over 2 to 5 levels. The ESP block produced additional spread to intercostal spaces over 5 to 9 levels andwasassociated with a greaterextent of craniocaudal spread along the paraspinal muscles.
Conclusions: The clinical effect of ESP and retrolaminar blocks can be explained by epidural and neural foraminal spread of local anesthetic. The ESP block produces additional intercostal spread, which may contribute to moreextensive analgesia. The implications of these cadaveric observations require confirmation in clinical studies.
(Reg Anesth Pain Med 2018;43: 756–762)
Theerector spinae plane (ESP) block is an ultrasound-guided regional anesthetic technique for analgesia of the thoracic andabdominalwall.1,2 It involves injection of local anesthetic into the musculofascial plane deep to the erector spinae muscles and superficial to the tips of the transverse processes. Cadaveric and
clinical evidence suggests that the local anesthetic may penetrate anteriorly through the intertransverse connective tissues into the paravertebral space where it acts on the ventral rami of spinal nerves1,2; local anesthetic may also reach and block the rami communicantes and sympathetic chain to produce visceral analgesia.3
It has been suggested4,5 that the ESP block is identical to an other paraspinal regional anesthesia technique, the retrolaminar block,6,7 which also involves injection into the musculofascial plane between the paraspinal muscles and underlying vertebrae.
Aswith the ESP block, it has been postulated that the clinical ef fects of the retrolaminar block may be explained by spread of local anesthetic into the paravertebral space,6 but this mechanism has never been systematically investigated. However, there are significant anatomical and technical differences between the 2 techniques: the retrolaminar block targets the lamina instead of the transverse process, and thus the injection point is more medial and deeper. The muscle layer over the lamina and adjacent to the
spinous processes is thicker, being composed of the spinalis portion of the erector spinae muscle group as well as the transversospinalis muscle group, which comprises the multifidus, rotatores, semis
pinalis, interspinalis, and intertransversarii muscles (Fig. 1). These differences can conceivably result in different patterns of local an esthetic spread, which may in turn have implications for their clinical effect. To examine if this was the case, we therefore performed a comparative study of injectate spread following the ESP block and retrolaminar block in fresh cadavers, using both magnetic res onance imaging (MRI) and anatomical dissection.
The study procedures were performed on 3 fresh human ca davers in the Multidisciplinary Lab of Penn State College of Medicine, Milton S. Hershey Medical Center, Hershey, Pennsylvania. The Institutional Review Board of Ethics of Penn State Hershey College of Medicine, Pennsylvania, approved the study for exemption from formal review.
Erector Spinae Plane and Retrolaminar Blocks
The same cadaver was used for both block techniques to minimize bias from varying body mass and tissue quality. Each cadaver was randomly allocated to receive an ESP block on either the left or right side of the body, and a retrolaminar block was per for medontheopposite side. Bothblockswere performed with the cadaver in a prone position and at the level of the T5 vertebra, which was identified using ultrasonography and a counting-down approach from the T1 transverse process–first rib junction. A 40-mL solution comprising 35 mL of 0.9% normal saline, 4 mL of methylene blue, and 1 m Lofgadopentetate dimeglumine (Magnevist; Bayer Health care LLC, Whippany, New Jersey) was prepared for each cadaver, and 20 mL of this solution was injected in each block. All injections were performed by an investigator with experience in both techniques (S.D.A.).
The ESP block was performed by placing a high-frequency (12–15 MHz) linear-array ultrasound transducer in a longitudinal parasagittal orientation over the tip of the transverse processes and inserting a 22-gauge 80-mm needle (Stimuplex Ultra 360; B. Braun, Bethlehem, Pennsylvania) in a caudal-to-cranial direction in plane with the ultrasound beam to contact the tip of the T5 transverse process. Correct needle tip position was confirmed by the injection of 0.5 to 1 mL of 0.9% normal saline and visualization of linear fluid spread that distended the fascial plane between the erector spinae muscle and the transverse process (Fig. 2). This was followed by in jection of 20 mL of the radiocontrast dye solution.
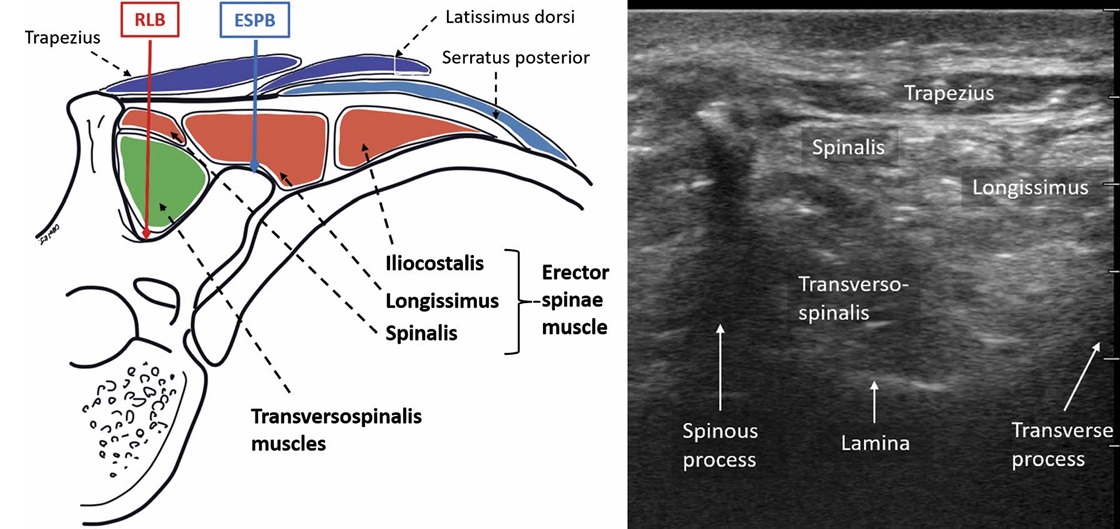
FIGURE 1. Schematic diagram of the muscles of the back in relation to a representative thoracic vertebra and rib, with accompanying ultrasound image. The superficial muscles include the trapezius, rhomboids (not shown), and latissimus dorsi. The erector spinae muscles comprise the intermediate layer, and the transversospinalis muscles (primarily multifidus, rotatores, and semispinalis) make up the deep layer. The location of injection with the retrolaminar (RLB) and ESP block (ESPB) are shown.
The retrolaminar block was also performed with the ultrasound transducer placed in a similar longitudinal parasagittal orientation but closer to the midline so as to image the laminae of the thoracic ver tebrae. The same needle was inserted in a cranial-to-caudal direction in plane with the ultrasound beam to contact the T5 lamina. Correct needle tip position was verified by injection of 0.5 to 1 mL of 0.9%normal saline and visualization of linear fluid spread between erector spinae muscle and the lamina(Fig. 2). Twenty milliliters of the radiocontrast-dye solution was then injected.
Magnetic Resonance Imaging Protocol
Within 30 to 45 minutes after completion of both injections, the cadaver was imaged in a supine position in a 3-T Siemens Magnetom Prisma Fit MRI scanner (Siemens, Washington, DC). Coronal isotropic 3-dimensional SPACE (Sampling Perfection with Application optimized Contrasts using different flip angle Evolution) images were acquired in T1 weighting (echo time, 11 milliseconds; repetition time, 600 milliseconds) with fat saturation and T2 weighting (echo time 248 milliseconds; repetition time, 2850 milliseconds) with fat saturation (T2FS). Axial and sagittal images were reconstructed from the coronal acquisitions. The images were interpreted by comparing the T1 and T2
sequences. The T2FS images were used to differentiate the injected contrast solution from thrombosed blood within the cadaveric vessels and tissues, both of which are hyperintense in signal on T1-weighted fat-saturated images. On the T2FS images, the injected contrast solution was imaged as a low-intensity signal, whereas the thrombosed blood remained hyperintense in signal. Images were interpreted by a musculoskeletal radiologist with 13 years of experience (S.B.). The radiologist was blinded as to which side received a retrolaminar versus ESP block. The maximum craniocaudal soft tissue distribution of injectate was re corded based on thevertebral level, and the tissue planes containing contrast were noted. The maximum medial-to-lateral distribution of injectate in the soft tissues was recorded in centimeters from the midline, measuring from the midspinous process on axial images. The neural foramina into which contrast entered was recorded,
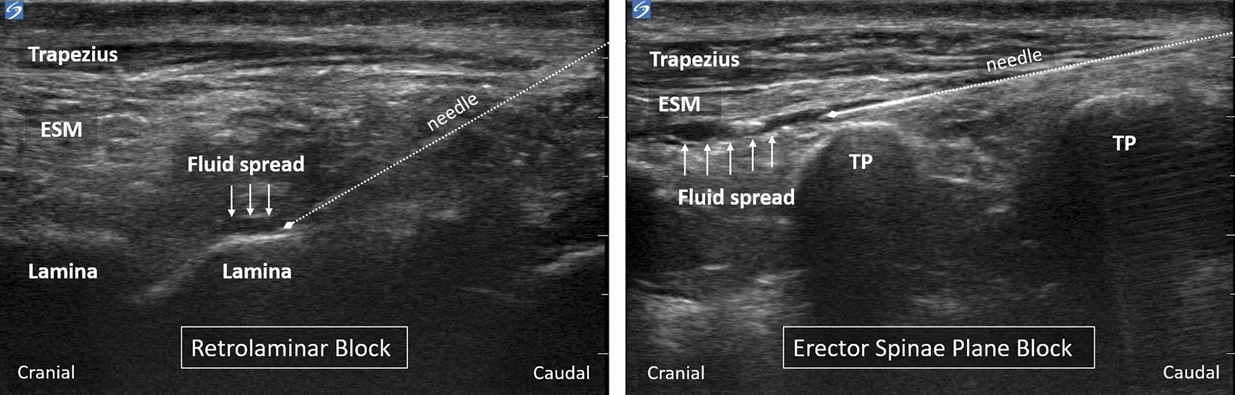
FIGURE 2. A parasagittal longitudinal view of the lamina or tip of the transverse processes (TP) is obtained for the retrolaminar and ESP blocks, respectively. In both blocks, the needle is advanced in plane to the ultrasound beam to enter the musculofascial plane between erector spinae muscle (ESM) and the bony surface. The end point is visible linear fluid spread that separates the ESM from the bony surface.
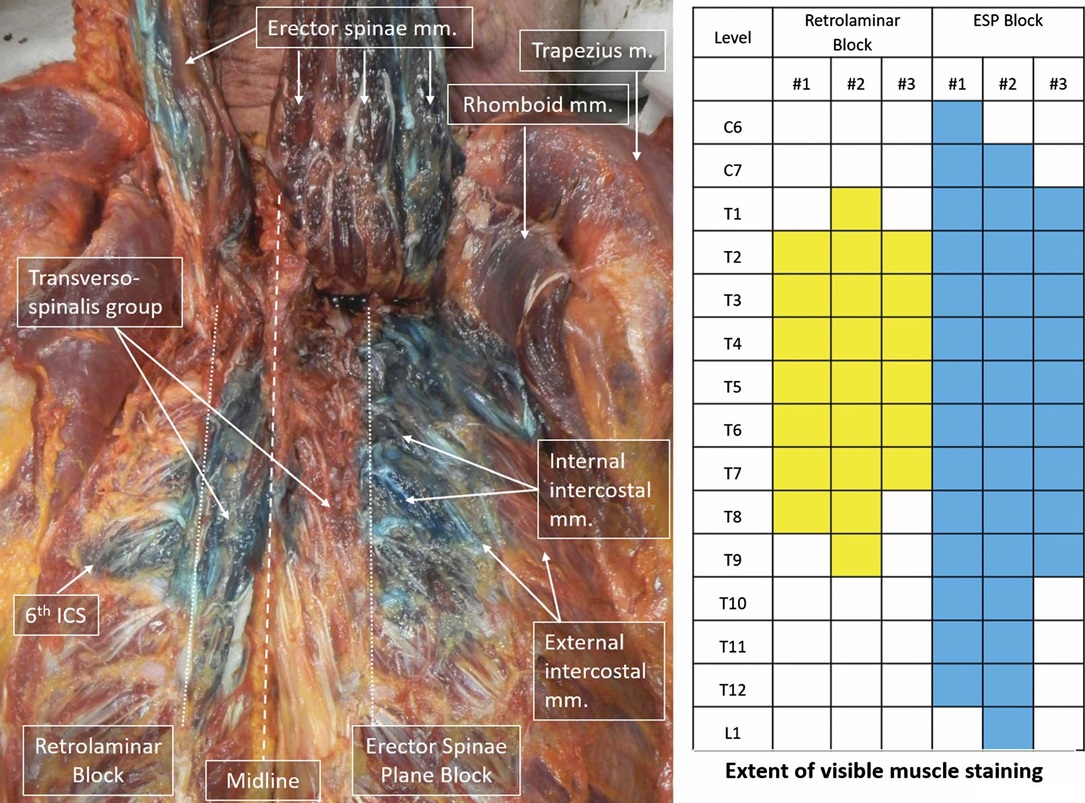
FIGURE 3. Anatomical dissection of cadaver 2 following retrolaminar and ESP block injections at T5. The trapezius and rhomboid muscles have been reflected laterally. The erector spinae muscles have been reflected superiorly, and dense staining is visible on the anterior surface. The ESP block has resulted in spread of injectate laterally into the intercostal spaces, whereas the distribution of the retrolaminar block is primarily confined to the transversospinalis group of muscles between the spinous processes (dashed line) and the tips of the transverse processes (dotted lines). The craniocaudal extent of visible staining of transversospinalis and erector spinae muscles on anatomical dissection is shown in the accompanying graphic.
as were the vertebral levels of cranial-caudal extension of contrast along the epidural space.
Anatomical Dissection
Anatomical dissection was performed with the cadavers in a prone position by a single anatomist (H.L.) whowas blinded as to which side received a retrolaminar versus ESP injection. The skin andsubcutaneoustissues over the back were removedbetween the
midaxillary line on each side and from the external occipital pro tuberance to the tip of the coccyx. The trapezius, latissimus dorsi, rhomboid major, rhomboid minor, and serratus posterior superior and inferior muscles were identified, detached from their medial attachments on the spinous processes, and reflected laterally. The thoracolumbar fascia was separated and removed from the posterior surface of the erector spinae muscle. At the midthoracic level, the 3 columns of the erector spinae (spinalis, longissimus, and iliocostalis) were separated using blunt dissection so as to de fine and identify them. These muscle columns were cut at the caudal end and reflected superiorly to visualize the thoracic cage and the muscles of the transversospinalis group. The transversospinalis group is the deep layer of the intrinsic back muscles that lie between the spinous and transverse processes. Five sets of muscles comprise this group: the multifidus, rotatores, semispinalis, interspinalis, and
intertransversarii. At each stage of the dissection, the extent of methylene blue dye staining was photographed and noted.
Anatomical dissection revealed that dye staining of the erector spinae and transversospinalis group of muscles was more extensive in the 3 hemithoraces that had received an ESP block versus the 3 that received a retrolaminar block. The craniocaudal extent of dye staining was greater following the ESP block (9, 14, and 14 ver tebral levels in each hemithorax) compared with the retrolaminar block (6, 7, and 9 levels) (Fig. 3). The medial-to-lateral extent of dye spread following the retrolaminar block was confined to the area between the spinous processes and the edge of the bony lamina, with the exception of cadaver 2, in which staining was observed extending 6 cm lateral to the midline in the sixth intercostal space (Fig. 3). In contrast, the ESP block produced less staining of the transversospinalis group of muscles adjacent to the midline, but there was consistent lateral spread into the intercostal spaces at mul
tiple levels following the ESP block (Fig. 3). In all 3 hemithoraces, the extent of this lateral dye staining was greatest at the fifth inter costal space, extending 9 to 10 cm lateral to the midline.
The MRI findings were consistent with that of anatomical dis section. The ESP block was associated with greater craniocaudal and medial-to-lateral distribution than the retrolaminar block (Fig. 4). The ESP block produced in jectate spread in the tissue planes around the erector spinae muscle and into the intercostal spaces (Fig. 5).
The number of intercostal spaces involved ranged from 5 to 9 (Fig. 6). Injectate spread following the retrolaminar block, on the
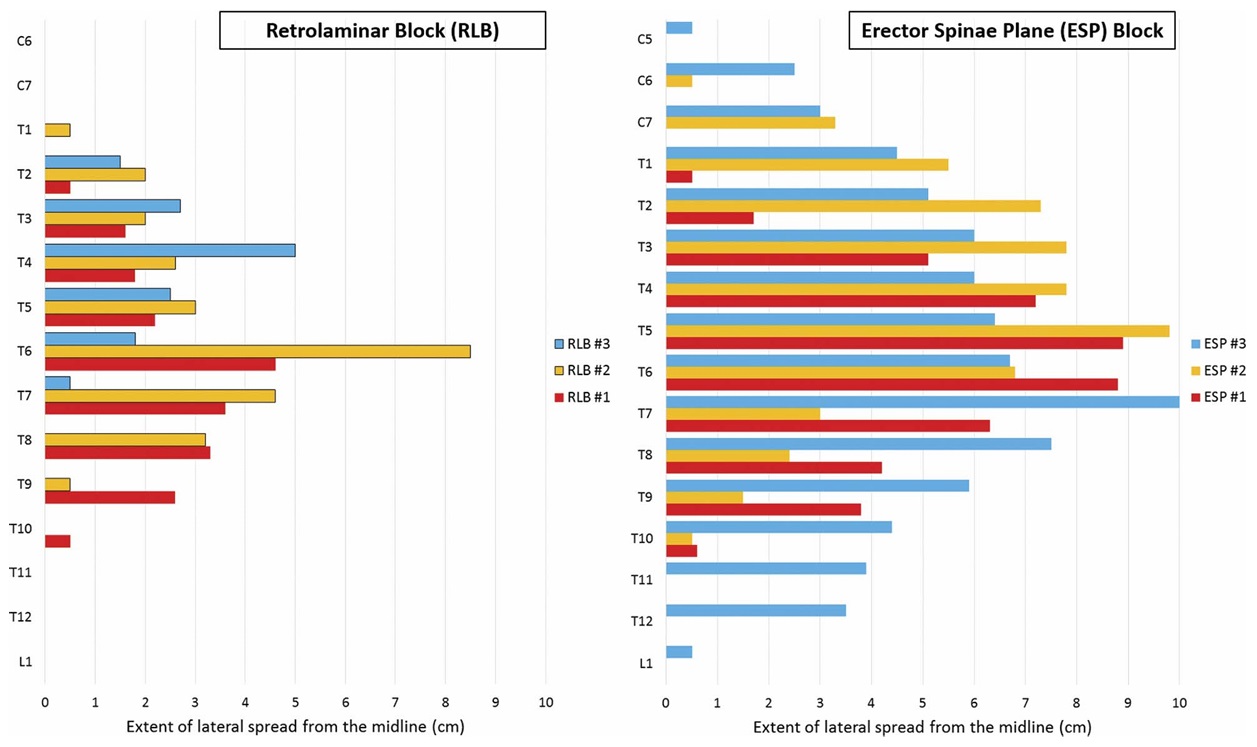
FIGURE4. Craniocaudal and medial-lateral extent of injectate spread on MRI following single-injection retrolaminar and ESP blocks at the T5 vertebral level. Each block was performed on 1 side of 3 cadavers, and the distribution observed in each hemithorax is illustrated.
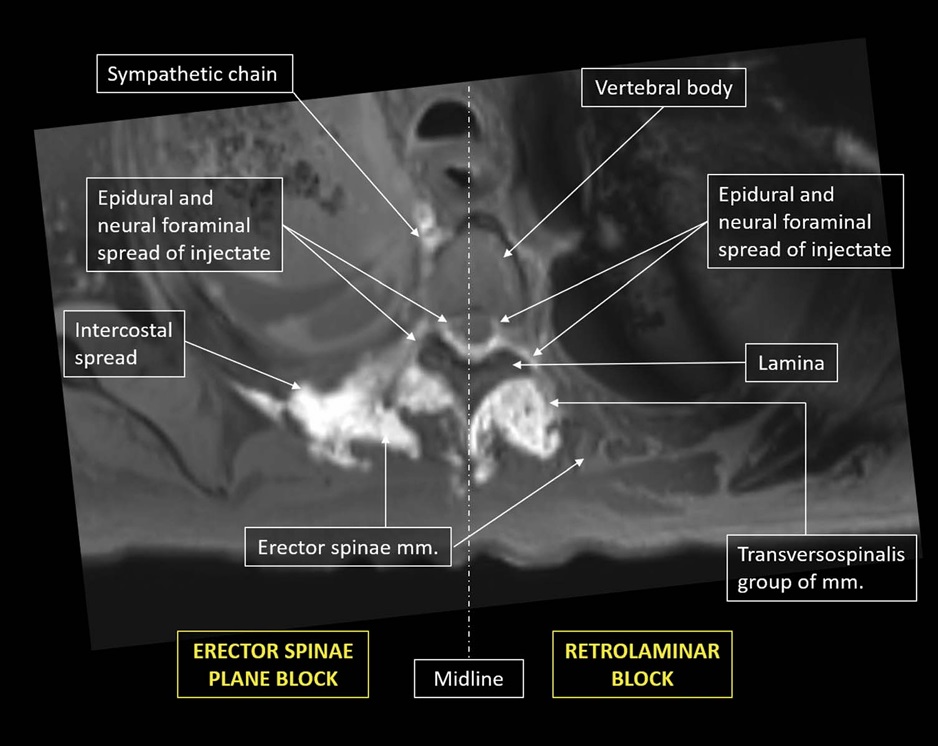
FIGURE 5. Axial MRI scan (T1-weighted with fat saturation). Injectate distribution following a retrolaminar block is confined mainly to the transversospinalis muscles, whereas the ESP block involves more of the erector spinae muscles. Both techniques result in spread to neural foramina and epidural space. The ESP block produces additional spread to the intercostal space.
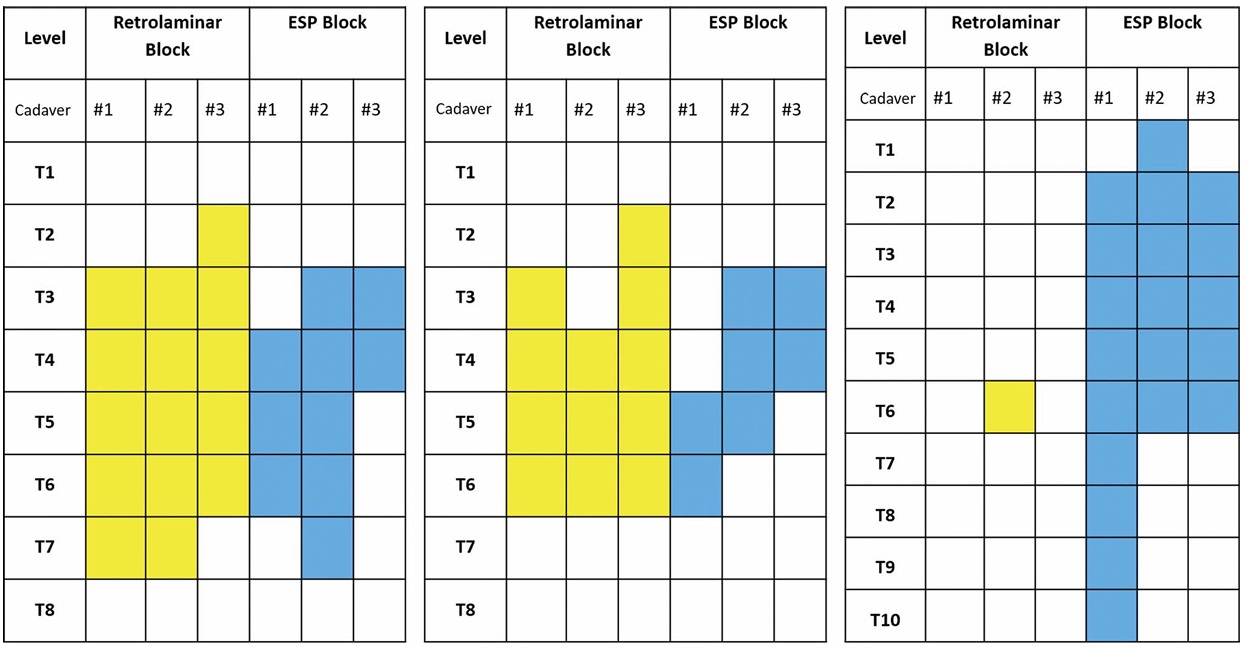
FIGURE 6. Distribution of visible spread on MRI to the epidural space, neural foramina, and intercostal space following single-injection retrolaminar and ESP blocks at the T5 vertebral level in each of the 3 cadavers.
other hand, was confined to the transversospinalis muscle group, except (as previously noted) in cadaver 2, where there was lateral spread in the sixth intercostal space.
There was visible injectate distribution to the neural foramina and epidural space with both techniques (Figs. 5 and 7). Epidural spread spanned 2 to 5 levels with the ESP block, and 5 levels con sistently with the retrolaminar block (Fig. 6). Injectate distribution
to neural foramina was somewhat less extensive than that in the epidural space, spanning 2 to 3 levels with the ESP block and 3 to 5 levels with the retrolaminar block (Fig. 6).
The results of our study reveal both significant similarities and differences between the distribution of injectate produced by the ESP block and retrolaminar block, which may have implications for clinical efficacy. There was spread to the neural foramina and epidural space with both techniques. This was seen across 2 to 5 vertebral levels centered around the level of injection and pro vides a basis for the somatic and visceral analgesia that has been reported.1–3,6–13 It also confirms the existence of anatomical path ways for anterior spread of local anesthetic. While the exact pathways have yet to be defined, they probably include the perforations in the intertransverse connective tissues through which the dorsal rami of spinal nerves and accompanying vessels emerge. The fact that epidural spread does occur raises the possibility of symptomatic hypotension following either technique. The incidence is unlikely to exceed that observed with thoracic paravertebral blockade, which has recently been estimated as ranging from 0.07% to 1.5% in adults14 and 0.006% to 0.3% in pediatric patients,15 but practitioners should remain vigilant. The observed pattern of spread with both retrolaminar and ESP blocks is in fact very similar to that described in imaging studies of thoracic paravertebral blockade using landmark-guided16,17 and ultrasound guided18 approaches. These have invariably demonstrated that injectate spreads beyond the paravertebral space into the epidural and intercostal spaces in a significant proportion of cases. Our findings lend further support to the presumption that retrolaminar and ESP blocks areviable al ternatives to thoracic paravertebral blockade8,9,13; however, comparative clinical studies are clearly required for confirmation.
Comparedwiththe retrolaminar block, the ESP block appears to have an additional mechanism of action for analgesia of the an terolateral thoracic and abdominal wall, namely, injectate spread into the intercostal spaces where local anesthetic can act on the ventral rami. This lateral distribution was not seen to any signifi cant extent with the retrolaminar block. This is probably due to the more medial site of injection and the fact that the target plane is deep to a thicker layer of muscle that may be more adherent to
the underlying laminae. Thiswould also explain the more restricted craniocaudal spread that was seen with the retrolaminar block. The ESP block stained the erector spinae muscle across a range of 9 to 14 vertebral levels compared with a range of 6 to 9 levels with the retrolaminar block. More importantly, the ESP block produced spread into up to 9 intercostal spaces from a single point of injection. This enhanced coverage allows for effective somatic analgesia in surgeries where incisions are widely spaced (such as thoracot omy with chest tube insertion9), multiple rib fractures,13 or where the surgical field or wound dressings prevent injection at a level congruent with the surgical site.11
Limitations of this study include the small sample size and the fact that it was performed in cadavers, albeit fresh ones. Post mortem changes in the integrity and permeability of tissues may influence fluid dispersion, and a similar study should ideally be performed in live subjects to confirm the findings as well as to document the extent of associated sensory block and analgesia. Studies of thoracic paravertebral block have shown that the radio graphic spread and sensory block distribution often correlate poorly, with the latter tending to be more extensive.17,18 Another caveat is that the observed epidural spread could have occurred because of spillover from the contralateral block technique; however, the fact
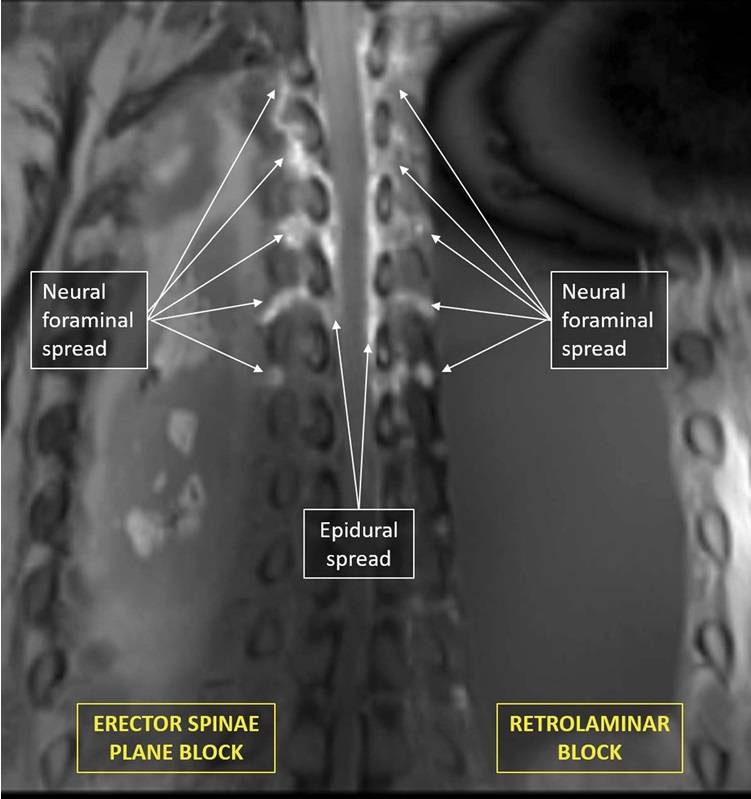
FIGURE 7. Coronal MRI scan (T1 weighted with fat saturation).Injectate distribution is visible in the region of the neural foramina and epidural space across multiple vertebral levels following both ESP and retrolaminar blocks.
that this spread was contiguous with ipsilateral neural foraminal and perimuscular spread makes this less likely.
We have established an anatomical basis for the clinical action of retrolaminar and ESP blocks and identified important differences between them. Single-injection retrolaminar and ESP blocks in fresh cadavers both produce epidural and neural foraminal spread across several levels that are centered around the level of injection and thus can be expected to have clinical effects similar to thoracic paravertebral blockade. The ESP block exhibits additional intercostal spread that may contribute to wider analgesic coverage than the retrolaminar block. This may be advanta geous in certain clinical scenarios. Randomized controlled trials in patients are required to explore the clinical implications of our observations.
1. Chin KJ, Adhikary S, Sarwani N, Forero M. The analgesic efficacy of
pre-operative bilateral erector spinae plane (ESP) blocks in patients having
ventral hernia repair. Anaesthesia. 2017;72:452–460.
2. Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae
plane block: a novel analgesic technique in thoracic neuropathic pain.
RegAnesthPainMed. 2016;41:621–627.
3. Chin KJ, Malhas L, Perlas A. The erector spinae plane block provides
visceral abdominal analgesia in bariatric surgery: a report of 3 cases.
RegAnesthPainMed. 2017;42:372–376.
4. Murouchi T. Consideration of block nomenclature: erector spinae
plane block or retrolaminar block? RegAnesthPainMed. 2017;42:124.
5. Ueshima H, Otake H. Similarities Between the retrolaminar and
erector spinae plane blocks. Reg Anesth Pain Med.2017;42:
123–124.
6. Voscopoulos C, Palaniappan D, Zeballos J, Ko H, Janfaza D, Vlassakov K.
The ultrasound-guided retrolaminar block. Can J Anesth. 2013;60:
888–895.
7. Jüttner T, Werdehausen R, Hermanns H, et al. The paravertebral lamina
technique: a new regional anesthesia approach for breast surgery.
JClinAnesth. 2011;23:443–450.
8. Murouchi T, Yamakage M. Retrolaminar block: analgesic efficacy and
safety evaluation. JAnesth. 2016;30:1003–1007.
9. Forero M, Rajarathinam M, Adhikary S, Chin KJ. Continuous erector
spinae plane block for rescue analgesia in thoracotomy after epidural
failure: a case report. A A Case Rep.2017;8:254–256.
10. Restrepo-Garces CE, Chin KJ, Suarez P, Diaz A. Bilateral continuous
erector spinae plane block contributes to effective postoperative analgesia
after major open abdominal surgery: a case report. A A Case Rep. 2017;9:
319–321.
11. Muñoz F, Cubillos J, Bonilla AJ, Chin KJ. Erector spinae plane block for
postoperative analgesia in pediatric oncological thoracic surgery.
Can JAnesth. 2017;64:880–882.
12. Forero M, Rajarathinam M, Adhikary S, Chin KJ. Erector spinae plane
(ESP) blockin the management ofpostthoracotomy pain syndrome: a case
series. Scand J Pain. 2017;17:325–329.
13. HamiltonDL,ManickamB.Erectorspinaeplaneblockfor painrelief inrib
fractures. Br J Anaesth. 2017;118:474–475.
14. Pace MM, Sharma B, Anderson-Dam J, Fleischmann K, Warren L,
Stefanovich P. Ultrasound-guided thoracic paravertebral blockade: a
retrospective study of the incidence of complications. Anesth Analg.2016;
122:1186–1191.
15. Vecchione T, Zurakowski D, Boretsky K. Thoracic paravertebral nerve
blocks in pediatric patients: safety and clinical experience. Anesth Analg.
2016;123:1588–1590.
16. Purcell-Jones G, Pither CE, Justins DM. Paravertebral somatic
nerve block: a clinical, radiographic, and computed
tomographic study in chronic pain patients. Anesth Analg. 1989;68:
32–39.
17. Naja MZ, Ziade MF, El Rajab M, El Tayara K, Lonnqvist PA. Varying
anatomical injection points within the thoracic paravertebral space: effect
on spread of solution and nerve blockade. Anaesthesia. 2004;59:459–463.
18. Marhofer D, Marhofer P, Kettner SC, et al. Magnetic resonance imaging
analysis of the spread of local anesthetic solution after ultrasound-guided
lateral thoracic paravertebral blockade: a volunteer study. Anesthesiology.
2013;118:1106–1112
