Objective: Historically, regional anesthesia for surgery on the posterior thoracic wall has been limited to neuraxial and paravertebral nerve blocks. The erector spinae plane (ESP) block is a novel technique that anesthetizes the dorsal rami of the spinal nerves innervating the posterior thoracic wall. We report the use of the ESP block for this clinical application in a pediatric patient.
Case Report: A healthy 3-year-old girl was scheduled for resection of a giant paraspinal lipoma extending over the T4–T7 dermatomes. She re ceiveda preoperative single-shot ESP block at the levelof the T1transverse process; this level was chosen to avoid the lipoma and cover the planned surgical incision over the T2–T8 dermatomes. Hemodynamic stability and excellent pain control perioperatively were obtained with minimal anesthetic requirements and no systemic analgesics apart from fentanyl administered for induction of anesthesia. Return to normal function (ambulation, feeding, and communication) was achieved within 2 hours after surgery. A pain score of 0 on the FLACC (Face, Legs, Activity, Cry, Consolability) scale was maintained until discharge from the hospital 4 hours after the surgery. First analgesic use was 18 hours after hospital discharge. No complications were reported.
Conclusions: The ESP block is an effective option for surgery on the posterior thoracic wall. The opioid- and anesthetic-sparing effects exhib ited in this case facilitated rapid postoperative recovery and early discharge.
(Reg Anesth Pain Med 2018;43: 217–219)
Regional anesthesia in pediatrics is a useful tool for pain man agement, and the application of ultrasound guidance has led to its increased use in this population.1 However, options for sur gery on the posterior thoracic wall have until now been limited to thoracic epidural or paravertebral blocks.2 The erector spinae plane (ESP) block is a novel technique that anesthetizes the dorsal rami of spinal nerve roots and thus the branches innervating the posterolateral thorax.3 There is only 1 report to date of its use for surgery of the posterolateral thorax in children.4 We de scribe our experience with the ESP block for excision of a large paraspinal lipoma in a 3-year-old patient.
Parental informed consent for publication was obtained. A healthy 3-year-old girl, 16 kg, was scheduled for resection of a giant dorsal lipoma as day-case surgery. The tumor was lo cated 2 cm lateral to the spine on the right side, measured 15 8cm,and extended over the T4–T7 dermatomes. Surgical incision was planned in a parasagittal plane over the right scapula (T2–T8 dermatomes). General anesthesia was induced with sevo
flurane, propofol 3 mg/kg, fentanyl 2 μg/kg, and rocuronium 0.6 mg/kg and maintained with sevoflurane (0.5 minimum alveo lar concentration) in an air-oxygen mixture. Following induction and intubation of the patient, an ultrasound-guided single-shot ESP block was performed for perioperative analgesia by an expe rienced pediatric regional anesthesiologist using an aseptic technique. The patient was turned into prone position. A high-frequency (7.5 MHz) linear transducer (7L5P; Shenzhen Mindray Bio Medical Electronics Co, Nanshan, China) was placed into a longi tudinal orientation over the tip of the transverse processes of T1 (Fig. 1). A 50-mm short-beveled needle (Sonoplex; Pajunk Medical Inc, Geisingen, Germany) was inserted craniocaudally in plane to
contact the tip of the transverse process beneath the fascia of the erector spinae muscle (Fig. 2). A 1:1 solution of bupivacaine 0.25% and lidocaine 1% was injected, and craniocaudal spread of local anesthetic (LA) was visually tracked with the transducer. This LA mixture is routinely used at our institution to ensure rapid onset of intraoperative analgesia. Spread of LA between the T1 and T9 transverse processes was achieved with a total volume of 0.2 mL/kg, at which point injection was stopped,

FIGURE 1. Photograph shows the transducer positioned lateral to the spine in a sagittal orientation and insertion of the needle in plane.
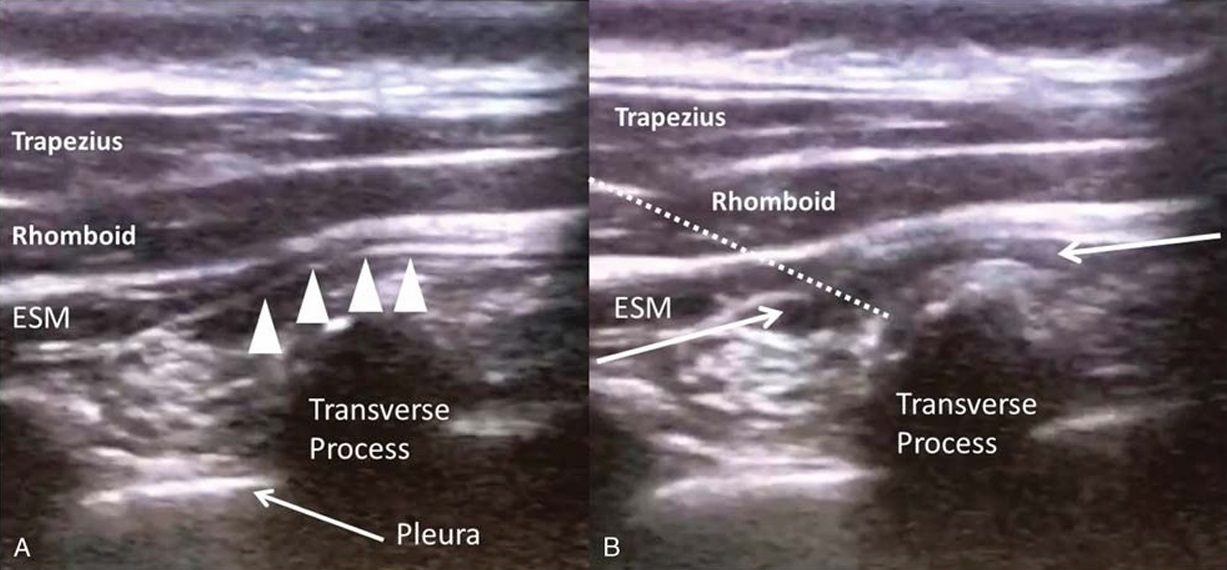
FIGURE 2. A, Ultrasound images of the erector spinae muscle (ESM) and its fascia (arrowheads), rhomboid and trapezius muscles, and transverse process.B,Ultrasound image showing injection of LAs underneath the erector spinae muscle fascia (arrows). Needle is shown in pointed line.
and the procedure concluded. Heart rate and blood pressure were stable within the age-appropriate reference range. Surgery lasted 2 hours, and emergence from anesthesia was uneventful. The patient was able to communicate, ambulate, and tolerate oral intake, with no evidence of pain (FLACC [Face, Legs, Activity, Cry,
Consolability] scale score of 0) 2 hours after the surgery. Assess mentofsen sory blockade was not possible because of the patient’s age. The patient was discharged home 4 hours after the surgery without further need for opioid analgesics or nonsteoridal anti inflammatory drugs perioperatively. Information and instructions
were provided to the mother about the offset of the block and subsequent pain management. Telephone follow-up was per formed 6 hours (the evening of the day of surgery) and 24 hours (the afternoon of postoperative day 1) after discharge. The patient requested and received a single dose of oral acetaminophen 20 mg/kg 18 hours after discharge.
The ESP block provides somatic and visceral analgesia by craniocaudal LA spread along the plane deep to the erector spinae muscle as well as anteriorly toward the paravertebral and intercostal spaces.3,5 Peripheral nerve blocks are associated with a lower rate of complications compared with neuraxial blocks.1,6,7 We be lieve that the relatively superficial nature of the ESP block, with the needle tip distant from the pleura and neuraxis, offers a superior risk profile compared with thoracic epidural or paravertebral analgesia, although it must be noted that there is insufficient published evidence for any definitive conclusions on safety.
A major advantage of the ESP block is its ability to cover multiple dermatomal levels from a single injection site.3 There fore, it can be performed, if necessary, at avertebral level different from the surgical site, to avoid wound dressings4 or surgical incision. In this case, we performed the block at the T1 vertebral level to avoid injecting through or close to the lipoma. Furthermore, our experience thus far in pediatric patients is that the spread of LA can be easily tracked with ultrasound, allowing us to deliver the
minimum volume required for the desired extent of coverage, reducing the risk of toxicity. This is an important advantage because there is no standardized dose for fascial plane blocks in children. Avolume of 0.2 mL/kg of LAwas highly effective and comparable with current analgesic data for fascial plane blocks in chil dren.6,8,9 We have been able to achieve adequate spread and analgesia with a volume of 0.2 to 0.3 mL/kg of LA in other pediatric patients undergoing thoracic surgery, and our results are in keeping with the analgesic efficacy of ESP block reported for thoracic spine surgery, thoracotomy, and rib fracture in the adult population.10–12 However, our case report has several limitations. First, because the patient went home at 4 hours after surgery, we only can report the time of first analgesic administration, not the full time course of pain scores. Therefore, we have only a rough estimation of the block’s analgesic duration. Second, our patient underwentsuperficial chest wall surgery, not a thoracotomy. With out controlled clinical trials, readers should not draw conclusions
about the possible effectiveness of erector spinae block for pediatric thoracotomy or thoracoscopy. In conclusion, this case demon strates the utility of the ESP block in providing analgesia for posterior superficial thoracic wall surgery.
ACKNOWLEDGMENTS
The authors thank Dr Cravero, who provided valuable input
for the study in the pediatric population.
1. Polaner DM, Taenzer AH, Walker BJ, et al. Pediatric Regional Anesthesia
Network (PRAN): a multi-institutional study of the use and incidence of
complications of pediatric regional anesthesia. Anesth Analg. 2012;115:
1353–1364.
2. Salviz EA, Akman N, Sivrikoz N, Demir K, Aydin A, Tugrul KM. An
exceptional indication for bilateral thoracic paravertebral block
performance in a pediatric patient. Agri. 2015;27:168–169.
3. Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae
plane block: a novel analgesic technique in thoracic neuropathic pain.
Reg Anesth Pain Med. 2016;41:621–627
4. Munoz F, Cubillos J, Bonilla AJ, et al. Erector spinae plane block for
postoperative analgesia in pediatric oncological thoracic surgery.
Can JAnesth.2017:10–12.
5. Chin KJ, Malhas L, Perlas A. The erector spinae plane block provides
visceral abdominal analgesia in bariatric surgery: a report of 3 cases.
RegAnesthPainMed. 2017;42:372–376.
6. Johr M. Regional anaesthesia in neonates, infants and children:
an educational review. Eur J Anaesthesiol. 2015;32:289–297.
7. Ecoffey C, Oger E, Marchand-Maillet F, Cimino Y, Rannou JJ, Beloeil H.
Complications associated with 27031 ultrasound-guided axillary brachial
plexus blocks. Eur J Anaesthesiol. 2014;31:606–610.
8. Suresh S, Taylor LJ, De Oliveira GS Jr. Dose effect of local anesthetics on
analgesic outcomes for the transversus abdominis plane (TAP) block in
children: a randomized, double-blinded, clinical trial. Paediatr Anaesth.
2015;25:506–510.
9. Hernandez MA, Vecchione T, Boretsky K. Dermatomal spread following
posterior transversus abdominis plane block in pediatric patients: our initial
experience. Paediatr Anaesth. 2017;27:300–304.
10. HamiltonDL,ManickamB.Erectorspinaeplaneblockfor painrelief inrib
fractures. Br J Anaesth. 2017;118:474–475.
11. Forero M, Rajarathinam M, Adhikary S, Chin KJ. Continuous erector
spinae plane block for rescue analgesia in thoracotomy after epidural
failure: a case report. A A Case Rep. 2017;8:254–256.
12. Ueshima H, Otake H. Clinical experiences of ultrasound-guided erector
spinae plane block for thoracic vertebra surgery. JClinAnesth.2017;
38:137.
