Background and Objectives: The femoral and obturator nerves are assumed to account for the primary nociceptive in nervation of the hip joint capsule. The fascia iliaca compartment block and the so-called in-1-block have been used in patients with hip fracture based on a presumption that local anesthetic spreads to anesthetize both the femoral and the obturator nerves. Evidence demonstrates that this presumption is unfounded, and knowledge about the analgesic effect of obturator nerve blockade in hip fracture patients presurgically is thus nonexistent. The objectives of this cadaveric study were to investigate the proximal spread of the injectate resulting from the admin istration of an ultrasound guided obturator nerve block and to evaluate the spread around the obturator nerve branches to the hip joint capsule.
Methods: Fifteen milliliters of methylene blue was injected into the interfascial plane between the pectineus and external obturator muscles in 7 adult cadavers. The spread of the injectate into the obturator canal and around the obturator and accessory obturator nerve branches to the hip joint was evaluated by subsequent dissection.
Results: The injected dye spread into the obturator canal and colored all obturator branches to the hip joint capsule in all 14 sides. Furthermore, the accessory obturator nerve was present in 3 sides (21%), and the nerve and its branches to the hip joint capsule were colored in all cases.
Conclusions: In cadavers, injection of 15 mL of methylene blue into the interfascial plane between the pectineus and the external obturator muscle effectively spreads proximally to reach the obturator canal, as well as the obturator nerve branches to the hip joint capsule and the accessory obturator nerve.
(Reg Anesth Pain Med 2017;42: 357–361)
Hip fractureis a painful condition with the majority of patients experiencing moderate to severe pain.1 In the literature, the fascia iliaca compartment block (FICB), the “3-in-1-block” and the femoral nerve block are the peripheral nerve block techniques commonly investigated in regard to alleviating preoperative pain in patients with hip fracture.2
The FICB and the 3-in-1-block have both previously beenre ported to anesthetize the obturator nerve, as well as the femoral andlateral femoral cutaneousnerves.3,4
These presumptions made such high-volume blocks the most appropriate nerve blocks for preoperative analgesia in patients with hip fracture, because both the femoral and obturator nerves have been found to innervate the hip joint capsule.5
Several authors have since questioned the reliability of the FICB and the 3-in-1-block to anesthetize the obturator nerve.6–10 Recently, a study, using magnetic resonance imaging to visualize the spread of the injectate, refuted any spread of local anesthetic to the obturator nerve after either of the 2 nerve block techniques.11
Consequently, knowledge of the analgesic effect of an obturator nerve block in preoperative patients with hip fracture is nonexis tent. To provide such knowledge,a selective obturator nerve block technique with documented spread of injectate around the obtura tor nerve and its branches innervating the hip joint capsule is warranted.
Different selective ultrasound-guided obturator nerve block techniques have been published within recent years.12–16 To the best of our knowledge, none of the previous studies of any ultrasound-guided technique, applicable to patients with hip frac ture, have investigated the proximal spread of the injectate into the obturator canal and around the obturator nerve branches innervating the hip joint capsule. Furthermore, no studies have investi gated spread of injectate to the accessory obturator nerve
(AON), which has been reported to innervate the hip joint capsule consistently, when present.17
The purpose of the present cadaveric study was to determine the proximal spread of the injectate into the obturator canal and around the obturator nerve and AON branches innervating the hip joint capsule after ultrasound-guided subpectineal injection.
Ultrasound-guided dye injections were carried out bilaterally in 7 cadavers (4 female and 3 male cadavers). They were donated to the Division of Clinical and Functional Anatomy of the Medical University of Innsbruck for scientific and educational purposes.18,19
All cadavers were preserved using an arterial injection of an ethanol-glycerol solution and immersion in phenolic acid in water for 1 to 3 months.20,21 The ultrasound scanning was performed using a high-frequency 13–4 MHz linear array probe (AL2442
probe, Esaote MyLab Seven US System; Esaote, Genoa, Italy). An ultrasound scan was carried out to visualize the optimal location for injection into the interfascial plane between the pectineus and external obturator muscles close to the inferior mar
gin of the superior pubic ramus. The details of the technique have been presented previously by Taha.16
A100-mm,22-gauge,short-bevel needle (Stimuplex D Plus; B.Braun,Melsungen,Germany)wasinsertedout-of-planeintothe fascial plane between the pectineus and external obturator muscles16 (Fig. 1, A and B). Fifteen milliliters of methylene blue (2%) was slowly injected interfascially using a 20-mL syringe (Fig. 1B). Subsequent to the injection, the cadaver was carefully dissected.
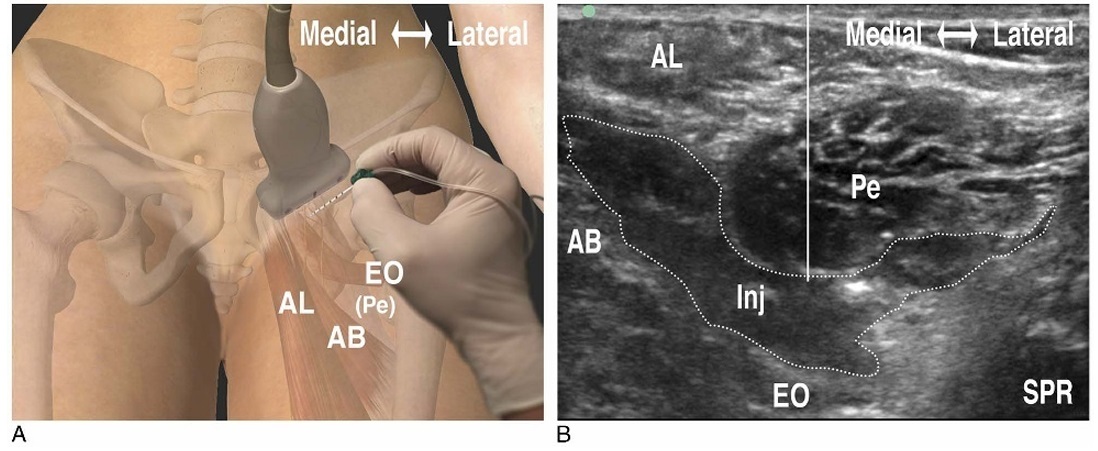
FIGURE 1. A, Transducer position and needle insertion point. AL indicates adductor longus muscle; AB, adductor brevis muscle; (Pe), pectineus muscle (faded); EO, external obturator muscle. The figure is a modified excerpt from Essential Anatomy 5, with permission from 3D4Medical(www.3d4medical.com).B,Ultrasonographicimageafter the subpectinealinjection on the left side. SPR indicates Superiorpubic ramus; solid white line, trajectory of the needle.
The injection was defined as successful for spread to the ob turator nerve, if the obturator branches to the hip joint capsule were colored by dye or if the dye did spread into the obturator canal, which contains the main trunk of the obturator nerve or the divisions. Successful spread to the AON was defined as coloring of the AON branches to the hip, when the AON was present, or al ternatively spread of the dye along the deep side of the pectineus muscle to its lateral margin at the attachment to the superior pubic ramus. After completion of each injection, the investigator who per formed the injection (T.F.B. or T.D.N.) left the dissecting room, and another investigator (B.M.), who was not present during the in jection, carried out the dissection and documented the spread of dye. Thesamedissection technique was performed in all 14 sides. This was performed immediately after injection of dye and as quickly as possible to avoid any distortion of results. Accordingly, the 2 initial incisions, 1 proximal incision slightly below the level of the inguinal ligament and a second medial incision along the gracilis muscle, went right through all epimuscular tissue layers. Subsequently, the tissue flap was raised and reflected laterally to expose the iliopsoas, pectineus, and adductor longus muscles, as well as the anterior border of the gracilis muscle. After resection of the superficial neurovascular structures and freeing the fascia covering the pectineus muscle and adductor longus, the gap be tween the 2 muscles was carefully widened to expose the deeper located adductor brevis muscle (Fig. 2A). Next, the pectineus muscle was transected near its distal attachment and reflected
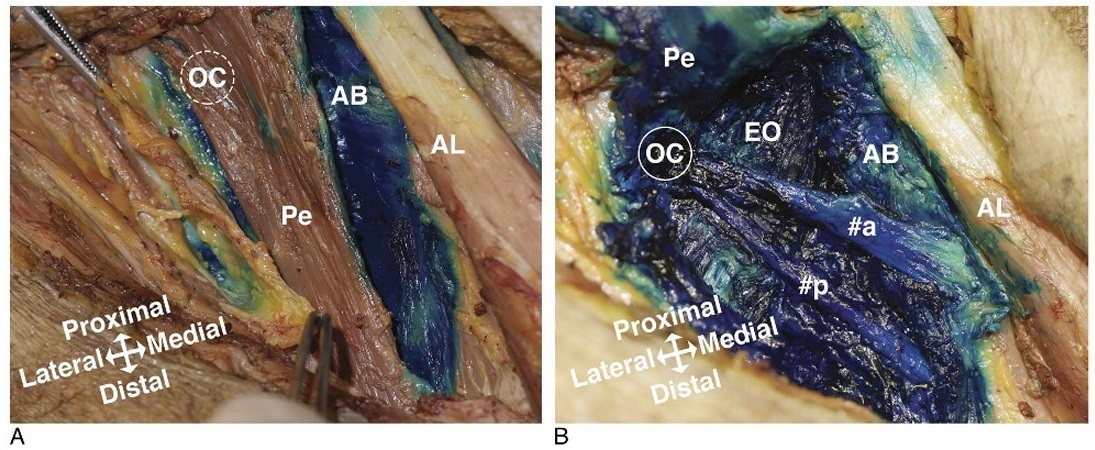
FIGURE 2. A, Exposure of the structures before transection and reflection of the pectineus muscle. OC indicates external orifice of the obturator canal (depiction of the deeper position); Pe, pectineus muscle; AB, adductor brevis muscle; AL, adductor longus muscle.
B, After reflection of the pectineus muscle, the anterior (#a) and posterior (#p) divisions of the obturator nerve are visible in their extrapelvic trajectory anterior to the external obturator muscle (EO).Note that the deep surface of the pectineus muscle is stained by methylene blue.
proximally, which exposed the obturator nerve (Fig. 2B). This allowed the obturator nerve to be inspected for perineural spread of dye by following it proximally toward the obturator canal, as well as distally both anteriorly and posteriorly to the adductor brevis muscle.
Finally, the hip articular branches of the obturator nerve, as well as the AON (if present), were identified and followed.
Ultrasonographic identification of the interfascial plane between the pectineus and external obturator muscles close to the inferior margin of the superior pubic ramus was feasible bilaterally in all cadavers. The injected methylene blue spread around
the obturator nerve branches to the hip joint in 14 of 14 dissected
sides (100%).
The methylene blue solution spread into the obturator canal and colored the trunk of the obturator nerve or its anterior and pos teri or divisions in 14 of 14 sides (100%).
In addition to spread of dye to the trunk or the divisions of the obturator nerve inside the obturator canal, both the anterior and posterior divisions were also colored in their extrapelvic trajectory by the injection in all cases (100%).
The AON was present in 3 of the 14 dissected sides (21%). In jectate surrounding the AON and its branches to the hip joint capsule was observed in all 3 cases (100%), and methylene blue spread along the deep side of the pectineus muscle to its lateral margin and the attachment tothe superior ramus of the pubic bone in all cases when the AON was not present (100%).
The present study of 7 cadavers (14 sides) demonstrated that ultrasound-guided injection of 15 mL of dye into the interfascial plane between the pectineus and external obturator muscles, close to the inferior margin of the superior pubic ramus, generates a
proximal spread of the injectate into the obturator canal and to the obturator nerve and AON branches to the hip joint capsule with a very high success rate.
The injected methylene blue spread around the AON when present and consistently spread along the deep side of the pectineus muscle to its lateral margin, where the AON lies when present.
The observed pattern of spread of dye aroundthe branches to the hip joint capsule from both the obturator nerve and AON pro vides evidence in support of the hypothesis that this ultrasound guided subpectineal single-injection technique would be effective for analgesia as a supplement to a femoral nerve block in patients with hip fracture prior to surgery.
The obturator nerve and the AON both originate from the anterior rami of lumbar plexus spinal nerves L2–L4 (Fig. 3). The variable presence of an AON is 1 of more reasons for the complexity of the innervation of the hip joint capsule. Birnbaum et al5 reported on the femoral nerve to innervate the anterolateral capsule and the obturator nerve to innervate the anteromedial cap sule. Combined innervation of the anterior capsule by 2 nerves was often observed. The posterior and inferior parts of the hip joint capsule were innervated by the sacral plexus. Innervation from the sacral plexus nerves consisted of branches directly from the sciatic or superior gluteal nerves or via the sciatic nerve branch to the quadratus femoris muscle.
A histological study of the hip joint capsule found nociceptive fibers to be predominantly present in the anterior and superolateral parts of the hip joint capsule. Neural fibers found in the posterior and inferior parts were identified as mechanore ceptors.23
These findings support the assumption that the femoral and obturator nerves are the primary mediators of pain in patients with hip fracture and may thus simplify the innervation of the hip joint capsule from the perspective of analgesia and regional anesthesia.
If these findings are correct, the contribution of this study to a validation of an ultrasound-guided obturator nerve block with spread of injectate to the hip articular branches holds the potential to improve preoperative analgesia in patients with hip fracture.
The present finding of spread of dye into the obturator canal is in good keeping with the result based on dissection of a single cadaver presented by Yoshida et al,24 who found a similar spread into the obturator canal by using a different technique, not applicable to patients with hip fracture. Yoshida et al24 did, however, tar get the same intermuscular space for the injection.
Acadaveric investigation of the proximal spread of injectate after a blind landmark-based injection technique has been con ducted previously by Feigl et al,25 who reported a success rate of
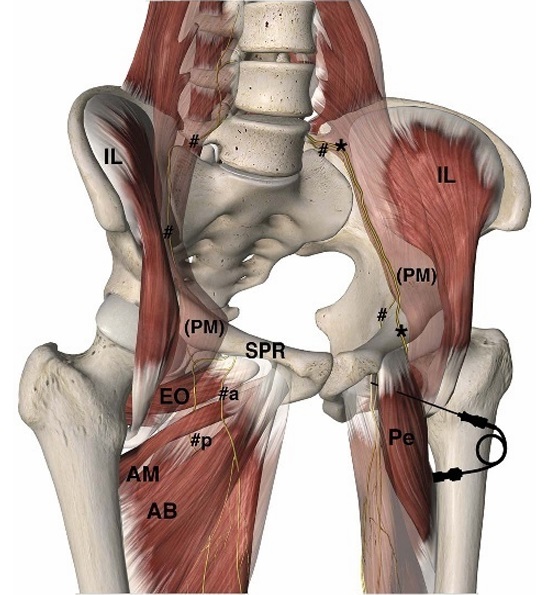
FIGURE3. The obturator nerve (#) and the AON (*) both originate from the anterior rami of lumbar plexus spinal nerves L2-L4, and both nerves descend along the medial side of the psoas major muscle (PM [faded]). The obturator nerve dives into the lesser pelvis and continues inferiorly to the superior pubic ramus (SPR) and reaches the obturator canal. It branches into an anterior (#a) and a posterior (#p) division, and the hip articular branches originate either from the main nerve trunk or its divisions.13 All obturator nerve branches leave the pelvis through the obturator canal. The AONI Iiesacrossthe uppersurfaceofthe superiorpubicramus and descends directly on the bone deep to the lateral side of the pectineus muscle (Pe).17,22 The AON has been reported to be
present in 13% of sides and, when present, always innervating the hip joint capsule.17IL indicates iliacmuscle; EO, external obturator muscle; AM, adductor magnus muscle; AB, adductor brevis muscle.
The pectineus muscle on the right side and the adductor longus muscle and psoas major muscle bilaterally are faded to make them transparent. The needle and point of injection, just deep to the pectineus muscle, are depicted on the left side. The figure is a
modified excerpt from Essential Anatomy 5, with permission from 3D4 Medical, San Diego, California.
93% in spread of dye to the trunk of the obturator nerve.However, these authors did not report on the frequency of spread of dye to the obturator canal or the branches to the hip joint capsule.
Previously, other authors have reported effective anesthesia of both the anterior and the posterior divisions of the obturator nerve, using an ultrasound-guided proximal single- injection tech nique in the interfascial plane between the pectineus and external obturator muscles.13,16 Our study supports the previously reported effect on both obturator nerve divisions. We observed spread into the obturator canal containing the main obturator nerve trunk or both its divisions. We also documented spread of dye to the ante rior and posterior nerve divisions in their extrapelvic trajectory. These findings support the feasibility of this injection technique, also when the indication is to block both of the obturator nerve di visions for more distal analgesic purposes. Total knee arthroplasty is probably the most obvious indication, because the anterior divi sion of the obturator nerve is believed sometimes to supplement the important sensory in nervation of the knee from the posterior division of the obturator nerve.26 Runge et al27 used the same proximal obturator nerve block technique in a randomized con trolled trial on postoperative pain after total knee arthroplasty and showed a significant reduction in morphine consumption when this obturator nerve block was added to a femoral nerve block.
The injection technique used in this study used transverse plane ultrasound imaging and an out-of-plane needle approach. The location of injection most probably corresponds to the loca tion described by Akkaya et al,12 who used a sagittal scanning technique. The transverse and sagittal approaches can be speculated to be equally effective.
The lumbar plexus block technique also approaches the obturator nerve sufficiently proximal to anesthetize the hip articular branches. In favor of this technique is primarily the concomitant blockage of the femoral nerve. Unfortunately, several issues make the lumbar plexus block less suitable than a more distal approach, including the level of expertise needed to conduct this plexus block without a high incidence of block failures. The predominant drawbackisthe need forlateral positioning of the patient, which is probably why a randomized controlled trial in patients with hip fracture has never been published. However, in experienced hands and in a selected sample of patients, this plexus block could prob ably improve preoperative analgesia in patients with hip fracture.
There are certain limitations to our study. First, the present study was conducted as a nonrandomized, nonblinded observa tional study with the implied limitations of this methodological design. Second, regarding the process of dissection, it can be spec ulated that the spread of methylene blue could be artifactually enhanced by the dissection itself. This potential bias is always a risk in this type of study, but it can be minimizedby meticulous dissection as described in Methods. Third, the spread of methylene blue in a cadaver does not necessarily correspond to the distribution pattern of local anesthetic in living human beings. Finally, the use of embalmed specimens may have facilitated spread of dye that deviates from spread of local anesthetic in the living, but also from spread of methylene blue in either fresh nonembalmed cadavers or cadavers preserved by other techniques. To the best of our knowledge, no existing literature compared the spread of methylene blue injected into cadavers preserved by different techniques. Clinical studies are needed to confirm the potential analgesic effect of a proximal obturator nerve block in patients with hip fracture and
other relevant indications.
We conclude from the results of this study of 7 cadavers that a single injection of 15 mL of methylene blue into the interfascial plane between the pectineus and external obturator muscles suc cess fully generated proximal spread of dye in to the obturator canal and successfully colored the obturator branches innervating the hip joint capsule. Furthermore, the dye colored the AON and its branches to the hip joint capsule.
Future clinical investigations are mandated to explore the clinical effect of an obturator nerve block as a supplement to a femoral nerve block in patients with hip fracture.
1. Morrison RS, Siu AL. A comparison of pain and its treatment in advanced
dementia and cognitively intact patients with hip fracture. JPainSymptom
Manage. 2000;19:240–248.
2. Ritcey B, Pageau P, Woo MY, Perry JJ. Regional nerve blocks for hip and
femoral neck fractures in the emergency department: a systematic review.
CJEM.2016;18:37–47.
3. Dalens B, Vanneuville G, Tanguy A. Comparison of the fascia iliaca
compartment block with the 3-in-1 block in children. Anesth Analg.1989;
69:705–713.
4. Winnie AP, Ramamurthy S, Durrani Z. The inguinal paravascular technic
of lumbar plexus anesthesia: the “3-in-1 block”. Anesth Analg.1973;52:
989–996.
5. Birnbaum K,Prescher A,Hessler S,HellerKD. The sensory innervation of
the hip joint—an anatomical study. Surg Radiol Anat. 1997;19:371–375.
6. Lang SA, Yip RW, Chang PC, Gerard MA. The femoral 3-in-1 block
revisited. JClinAnesth.1993;5:292–296.
7. MarhoferP, NaselC,Sitzwohl C,KapralS.Magneticresonanceimaging of
the distribution of local anesthetic during the three-in-one block. Anesth
Analg. 2000;90:119–124.
8. Parkinson SK, Mueller JB, Little WL, Bailey SL. Extent of blockade
with various approaches to the lumbar plexus. Anesth Analg. 1989;68:
243–248.
9. Dolan J, Williams A, Murney E, Smith M, Kenny GN. Ultrasound guided
fascia iliaca block: a comparison with the loss of resistance technique.
Reg Anesth Pain Med. 2008;33:526–531.
10. Capdevila X, Biboulet P, Bouregba M, Barthelet Y, Rubenovitch J, d’Athis
F. Comparison of the three-in-one and fascia iliaca compartment blocks in
adults: clinical and radiographic analysis. Anesth Analg. 1998;86:
1039–1044.
11. Swenson JD, Davis JJ, Stream JO, Crim JR, Burks RT, Greis PE. Local
anesthetic injection deep to the fascia iliaca at the level of the inguinal
ligament: the pattern of distribution and effects on the obturator nerve.
JClinAnesth. 2015;27:652–657.
12. Akkaya T, Ozturk E, Comert A, et al. Ultrasound-guided obturator nerve
block: a sonoanatomic study of a new methodologic approach. Anesth
Analg. 2009;108:1037–1041.
13. Anagnostopoulou S, Kostopanagiotou G, Paraskeuopoulos T, Chantzi C,
Lolis E, Saranteas T. Anatomic variations of the obturator nerve in the
inguinal region: implications in conventional and ultrasound regional
anesthesia techniques. Reg Anesth Pain Med.2009;34:33–39.
14. Lee SH, Jeong CW, Lee HJ, Yoon MH, Kim WM. Ultrasound guided
obturator nerve block: a single interfascial injection technique. JAnesth.
2011;25:923–926.
15. Sinha SK, Abrams JH, Houle TT, Weller RS. Ultrasound-guided obturator
nerve block: an interfascial injection approach without nerve stimulation.
RegAnesthPainMed. 2009;34:261–264.
16. Taha AM. Brief reports: ultrasound-guided obturator nerve block: a
proximal interfascial technique. Anesth Analg. 2012;114:236–239.
17. Katritsis E, Anagnostopoulou S, Papadopoulos N. Anatomical
observations on the accessory obturator nerve (based on 1000 specimens).
Anat Anz. 1980;148:440–445.
18. McHanwell S, Brenner E, Chirculescu ARM, et al. The legal and ethical
framework governing body donation in Europe—a review of current
practice and recommendations for good practice. Eur J Anat.2008;12:
1–24.
19. Riederer BM, Bolt S, Brenner E, et al. The legal and ethical framework
governing body donation in Europe—1st update on current practice.
Eur J Anat.2012;16:1–21.
20. Kessler J, Moriggl B, Grau T. Ultrasound-guided regional anesthesia: learning
with an optimized cadaver model. Surg Radiol Anat. 2014;36:383–392.
21. Platzer W, PutzR,Pousel S.Newsystemfor thepreservation andstorage of
anatomical matter [in German]. Acta Anat. 1978;102:60–67.
22. Woodburne RT. The accessory obturator nerve and the innervation of the
pectineus muscle. Anat Rec. 1960;136:367–369.
23. Gerhardt M, Johnson K, Atkinson R, et al. Characterisation and
classification of the neural anatomy in the human hip joint. Hip Int.
2012;22:75–81.
24. Yoshida T, Onishi T, Furutani K, Baba H. A new ultrasound-guided pubic
approach for proximal obturator nerve block: clinical study and cadaver
evaluation. Anaesthesia. 2016;71:291–297.
25. Feigl GC, Ulz H, Pixner T, Dolcet C, Likar R, Sandner-Kiesling A.
Anatomical investigation of a new vertical obturator nerve block technique.
Ann Anat. 2013;195:82–87.
26. Bendtsen TF, Moriggl B, Chan V, Borglum J. The optimal analgesic block
for total knee arthroplasty. Reg Anesth Pain Med. 2016;41:711–719.
27. Runge C, Borglum J, Jensen JM, et al. The analgesic effect of obturator
nerve block added to a femoral triangle block after total knee
arthroplasty: a randomized controlled trial. Reg Anesth Pain Med.
2016;41:445–451.
